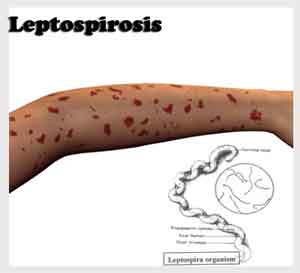
Leptospirosis is a bacterial infection that affects both humans and animals, caused by the Leptospira bacteria. It is prevalent worldwide, particularly in tropical and subtropical regions, and poses significant health risks if not promptly diagnosed and treated.
Causes and Transmission of Leptospirosis
The primary mode of transmission is through direct or indirect contact with the urine of infected animals. Common carriers include livestock such as cows and pigs, domestic pets like dogs, rodents, and various wild animals. The bacteria can survive in contaminated water or soil for weeks to months, increasing the risk of infection during activities involving exposure to these environments. Human infection typically occurs through.
- Contact with Contaminated Water or Soil: Engaging in activities such as swimming, wading, or working in environments contaminated with infected animal urine.
- Direct Exposure to Infected Animals: Handling animals or animal products without proper protective measures.
- Consumption of Contaminated Food or Water: Ingesting food or water that has been tainted with the bacteria.
It’s important to note that human-to-human transmission is rare.
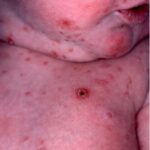
Recognizing the Symptoms of Leptospirosis
Leptospirosis manifests with a broad range of symptoms, often resembling other illnesses, which can complicate diagnosis. The incubation period ranges from 2 to 30 days, with most cases presenting after 5 to 14 days. Common symptoms include:
- Fever and Chills: Sudden onset of high fever accompanied by chills.
- Headache and Muscle Aches: Severe headaches and muscle pain, particularly in the calves and lower back.
- Gastrointestinal Distress: Nausea, vomiting, diarrhea, and abdominal pain.
- Jaundice: Yellowing of the skin and eyes, indicating liver involvement.
- Conjunctival Suffusion: Redness of the eyes without significant discharge.
In severe cases, complications may arise, such as kidney or liver failure, meningitis, respiratory distress, or even death if untreated.
Diagnosis and Treatment Strategies
Early diagnosis is crucial for effective treatment. Healthcare providers typically rely on a combination of clinical evaluation and laboratory tests, including blood tests to detect the presence of Leptospira bacteria or antibodies.
Treatment primarily involves antibiotics to eradicate the infection. For mild cases, oral antibiotics such as doxycycline or amoxicillin are commonly prescribed. Severe infections may necessitate intravenous administration of penicillin or ceftriaxone. Supportive care, including hydration and pain management, is also essential to aid recovery.
Preventative Measures to Reduce Risk
Implementing preventive strategies is vital to minimize the risk of leptospirosis:
- Avoid Contact with Potentially Contaminated Water: Refrain from swimming or wading in water bodies that might be contaminated, especially after heavy rainfall or flooding events.
- Protective Clothing: Wear appropriate protective gear, such as gloves and boots, when handling animals or working in environments at risk for contamination.
- Rodent Control: Implement measures to control rodent populations in residential and work areas to reduce exposure risk.
- Vaccination: Vaccinate domestic animals, particularly dogs, to prevent them from contracting and spreading the disease.
- Hygiene Practices: Maintain good hygiene by washing hands thoroughly after handling animals or soil and ensuring that food and water are sourced from safe, uncontaminated supplies.
Global Impact and Epidemiology
Leptospirosis is a significant global health concern, with an estimated one million cases occurring annually, resulting in approximately 60,000 deaths. The disease is more prevalent in tropical and subtropical regions due to favorable environmental conditions for the bacteria. Outbreaks are often associated with climatic events such as hurricanes and floods, which facilitate the spread of the bacteria through contaminated water sources.
Leptospirosis remains a critical public health issue worldwide. Understanding its transmission, recognizing early symptoms, and implementing effective prevention and treatment strategies are essential steps in reducing its impact. By promoting awareness and encouraging proactive measures, we can mitigate the risks associated with this potentially severe disease.