Leishmaniasis is a parasitic disease caused by protozoa of the Leishmania genus. Transmitted through the bites of infected female phlebotomine sandflies, this disease affects millions worldwide, particularly in tropical and subtropical regions. Leishmaniasis manifests in different forms, primarily cutaneous, mucocutaneous, and visceral leishmaniasis, each varying in severity and clinical presentation.

Causes and Transmission
Leishmaniasis is caused by over 20 species of the Leishmania parasite. The disease is primarily spread through:
- Sandfly Bites: Infected sandflies introduce the parasite into human or animal hosts.
- Animal Reservoirs: Rodents, dogs, and wild mammals serve as natural reservoirs for Leishmania.
- Human-to-Human Transmission: In rare cases, transmission occurs through blood transfusions, organ transplants, or congenital transmission.
Types of Leishmaniasis
1. Cutaneous Leishmaniasis (CL)
- Most common form
- Causes skin ulcers, nodules, or scaly lesions
- Lesions may take months to heal, leaving scars
- Common in the Middle East, South America, and the Mediterranean
2. Mucocutaneous Leishmaniasis (MCL)
- Affects mucous membranes of the nose, mouth, and throat
- Can lead to severe tissue destruction
- Found in South and Central America
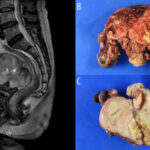
3. Visceral Leishmaniasis (VL) (Kala-Azar)
- Most severe form, potentially fatal if untreated
- Symptoms include fever, weight loss, anemia, and enlarged spleen/liver
- Prevalent in South Asia, East Africa, and Brazil
Symptoms of Leishmaniasis
- Cutaneous Leishmaniasis: Skin ulcers, sores, painless nodules
- Mucocutaneous Leishmaniasis: Nasal congestion, difficulty swallowing, facial disfigurement
- Visceral Leishmaniasis: Fever, night sweats, extreme fatigue, swollen liver and spleen
Diagnosis
- Microscopic Examination: Parasite detection in skin or tissue samples
- Polymerase Chain Reaction (PCR): DNA analysis for precise identification
- Serological Tests: Detect antibodies in blood (useful for VL diagnosis)
- Leishmanin Skin Test (Montenegro Test): Evaluates prior exposure
Treatment Options
1. Antimonial Drugs
- Sodium Stibogluconate (SSG) and Meglumine Antimoniate
- Used in VL and CL treatment, but with potential toxicity
2. Amphotericin B
- Liposomal Amphotericin B is the first-line treatment for VL
- Highly effective but requires intravenous administration
3. Miltefosine
- First oral drug for leishmaniasis treatment
- Effective against VL, CL, and MCL
4. Paromomycin
- An alternative for VL treatment, often used in combination therapy
Prevention Strategies
- Vector Control: Use of insecticide-treated bed nets and indoor spraying
- Protective Clothing: Covering exposed skin to prevent bites
- Environmental Management: Reducing sandfly breeding sites
- Vaccination Research: Ongoing trials for a potential vaccine
Global Burden and Epidemiology
- Over 1 million new cases of cutaneous leishmaniasis reported annually
- Visceral leishmaniasis has a fatality rate of nearly 95% if untreated
- Endemic in over 90 countries, including India, Brazil, Sudan, and Afghanistan
Leishmaniasis remains a significant public health concern, particularly in underserved regions. Early detection, prompt treatment, and effective vector control measures are crucial in reducing disease burden. Increased awareness and research efforts are essential to developing new treatment options and preventive measures to combat this neglected tropical disease effectively.