Left ventricular dysfunction (LVD) is a common and severe complication following a myocardial infarction (MI), also known as a heart attack. It occurs when the left ventricle (LV), the heart’s main pumping chamber, is unable to contract effectively, reducing cardiac output and increasing the risk of heart failure, arrhythmias, and sudden cardiac death. The degree of dysfunction depends on the extent of myocardial damage and the adaptive mechanisms of the heart.
Pathophysiology: How Myocardial Infarction Leads to LV Dysfunction
1. Myocardial Ischemia and Infarction
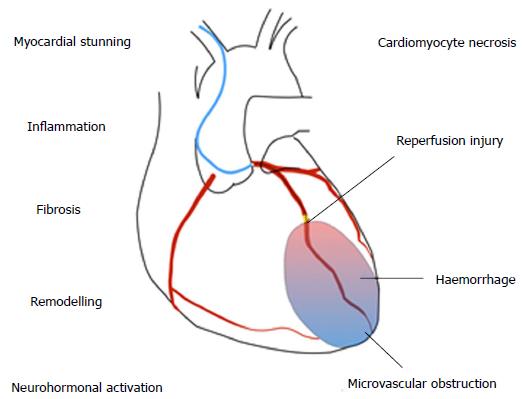
An MI results from the occlusion of a coronary artery, leading to ischemia (lack of oxygen) and necrosis of heart muscle cells. The affected myocardium loses its contractile function, weakening the heart’s ability to pump blood.
2. Ventricular Remodeling and Structural Changes
Following an MI, the heart undergoes ventricular remodeling, a process of structural and functional changes that may include:
✔️ Dilatation of the left ventricle (eccentric hypertrophy)
✔️ Fibrosis and scarring of infarcted tissue
✔️ Thinning of myocardial walls, reducing contractility
✔️ Increased left ventricular end-diastolic volume (LVEDV), leading to higher wall stress
3. Neurohormonal Activation and Hemodynamic Effects
The body attempts to compensate for reduced cardiac output through neurohormonal activation, triggering the renin-angiotensin-aldosterone system (RAAS) and sympathetic nervous system (SNS). While these mechanisms temporarily support blood pressure and perfusion, they ultimately contribute to hypertension, fluid retention, and further myocardial damage.
Clinical Manifestations of Left Ventricular Dysfunction
1. Symptoms
Patients with post-MI LV dysfunction may experience:
✔️ Dyspnea (shortness of breath) due to pulmonary congestion
✔️ Fatigue and exercise intolerance from reduced cardiac output
✔️ Peripheral edema resulting from fluid retention
✔️ Paroxysmal nocturnal dyspnea (PND) and orthopnea
✔️ Palpitations and arrhythmias
2. Complications
✔️ Heart Failure with Reduced Ejection Fraction (HFrEF): LV ejection fraction (LVEF) < 40%
✔️ Ventricular arrhythmias and sudden cardiac arrest
✔️ Left ventricular thrombus formation increasing stroke risk
✔️ Mitral regurgitation due to ventricular dilation affecting valve function
Diagnosis of Left Ventricular Dysfunction
1. Echocardiography (ECHO)
✔️ Assesses left ventricular ejection fraction (LVEF)
✔️ Detects regional wall motion abnormalities
✔️ Evaluates LV dilation and hypertrophy
2. Cardiac Magnetic Resonance Imaging (CMR)
✔️ Provides detailed imaging of myocardial scarring and fibrosis
✔️ Differentiates viable from non-viable myocardium
3. Electrocardiography (ECG)
✔️ Identifies prior infarction Q waves, ST-T changes, and conduction abnormalities
✔️ Detects ventricular arrhythmias
4. Biomarkers (Blood Tests)
✔️ Brain Natriuretic Peptide (BNP) or NT-proBNP: Indicates heart failure severity
✔️ Troponins: Confirms ongoing myocardial injury
✔️ Serum electrolytes and kidney function tests: Assesses systemic effects of heart failure
5. Cardiac Catheterization and Coronary Angiography
✔️ Evaluates coronary artery disease (CAD)
✔️ Determines viability of revascularization procedures
Management and Treatment Strategies
1. Pharmacological Therapy
| Drug Class | Mechanism | Clinical Benefits |
|---|---|---|
| ACE Inhibitors (e.g., Lisinopril) | Reduces afterload and inhibits RAAS | Prevents remodeling, lowers mortality |
| Beta-Blockers (e.g., Metoprolol, Carvedilol) | Decreases heart rate and myocardial oxygen demand | Improves survival, reduces arrhythmia risk |
| Aldosterone Antagonists (e.g., Spironolactone) | Blocks aldosterone-induced sodium retention | Reduces hospitalization, improves LV function |
| SGLT2 Inhibitors (e.g., Dapagliflozin) | Improves cardiometabolic function | Reduces cardiovascular mortality in heart failure |
2. Device-Based Therapies
✔️ Implantable Cardioverter Defibrillator (ICD): Prevents sudden cardiac death in patients with LVEF <35%
✔️ Cardiac Resynchronization Therapy (CRT): Improves cardiac output in patients with ventricular dyssynchrony
✔️ Left Ventricular Assist Devices (LVADs): Used in advanced cases as a bridge to heart transplantation
3. Surgical and Interventional Approaches
✔️ Revascularization (Percutaneous Coronary Intervention [PCI] or Coronary Artery Bypass Grafting [CABG]): Improves myocardial blood supply
✔️ Mitral Valve Repair/Replacement: Treats secondary mitral regurgitation
✔️ Ventricular Reconstruction Surgery: Reduces LV volume in severe cases
4. Lifestyle and Cardiac Rehabilitation
✔️ Regular physical activity: Improves cardiovascular fitness
✔️ Dietary modifications: Low sodium, heart-healthy diet
✔️ Smoking cessation and alcohol moderation
Prognosis and Long-Term Outlook
The prognosis of left ventricular dysfunction following myocardial infarction depends on early intervention, adherence to therapy, and overall cardiac function. Patients with well-managed LV dysfunction and LVEF stabilization have a better outlook, while those with progressive heart failure and recurrent ischemic events face higher mortality risks. Close monitoring, optimized medical therapy, and lifestyle changes are crucial for improving long-term survival.
Left ventricular dysfunction after a myocardial infarction significantly impacts cardiac function and quality of life. Early diagnosis, aggressive management, and evidence-based therapies can reduce complications and improve survival rates. Advances in pharmacological, device-based, and surgical interventions continue to enhance outcomes for affected patients.

