Large granular lymphocytic leukemia (LGL leukemia) is a rare hematologic malignancy characterized by an abnormal increase in large granular lymphocytes. It primarily affects T cells (T-LGL leukemia) or natural killer (NK) cells (NK-LGL leukemia) and often presents as a chronic condition with a slow progression.
Types of Large Granular Lymphocytic Leukemia
LGL leukemia is categorized into two main subtypes based on the type of lymphocyte involved:
- T-cell Large Granular Lymphocytic Leukemia (T-LGL): Accounts for 85% of cases and is associated with autoimmune disorders.
- Natural Killer Cell Large Granular Lymphocytic Leukemia (NK-LGL): Less common and can be aggressive or chronic.
Causes and Risk Factors
The exact cause of LGL leukemia remains unclear, but several factors have been linked to its development:
- Autoimmune disorders: Strong association with rheumatoid arthritis (RA) and other immune-mediated conditions.
- Genetic mutations: Somatic mutations in the STAT3 and STAT5B genes are frequently observed.
- Viral infections: Epstein-Barr virus (EBV) and human T-cell leukemia virus (HTLV) have been implicated in some cases.
- Environmental exposures: Prolonged exposure to toxic chemicals and radiation may contribute.
Symptoms of LGL Leukemia
LGL leukemia is often indolent but may cause symptoms due to immune dysregulation and cytopenias:
- Persistent neutropenia (low neutrophil count) leading to recurrent infections
- Anemia causing fatigue, weakness, and pallor
- Enlarged spleen (splenomegaly)
- Unexplained weight loss
- Joint pain and symptoms of rheumatoid arthritis
Diagnosis and Diagnostic Criteria
A definitive diagnosis of LGL leukemia involves a combination of laboratory tests and clinical findings:
1. Blood Tests
- Complete Blood Count (CBC): Shows neutropenia, anemia, and lymphocytosis.
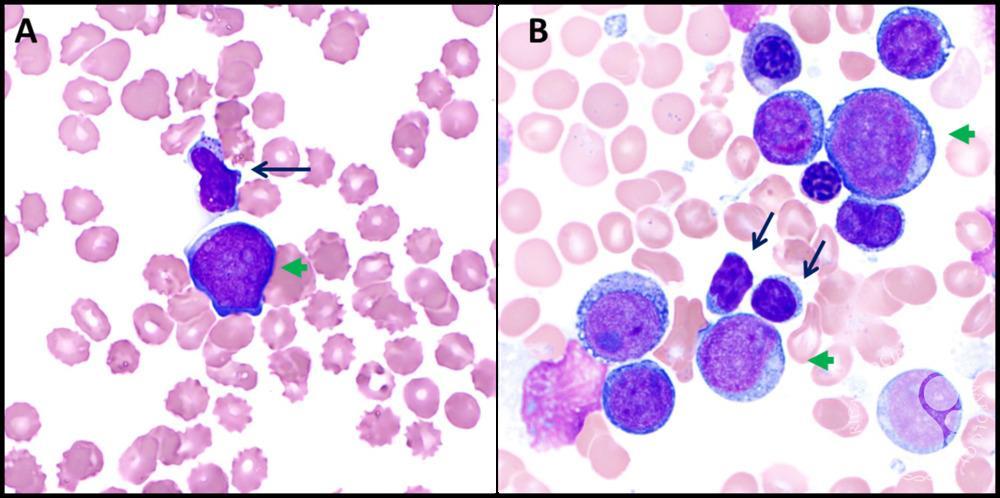
- Peripheral Blood Smear: Identifies large granular lymphocytes.
- Flow Cytometry: Confirms T-cell or NK-cell origin.
2. Bone Marrow Biopsy
- Reveals infiltration by abnormal lymphocytes.
- Helps rule out other hematologic malignancies.
3. Molecular and Genetic Testing
- STAT3 and STAT5B mutation analysis.
- T-cell receptor (TCR) gene rearrangement to confirm clonality.
Treatment Options for LGL Leukemia
LGL leukemia treatment depends on symptom severity and associated complications. Not all patients require immediate therapy.
1. Watchful Waiting
- Asymptomatic patients with stable blood counts may not require treatment.
2. Immunosuppressive Therapy
- Methotrexate: First-line therapy for symptomatic LGL leukemia.
- Cyclophosphamide or Cyclosporine: Used for refractory cases.
3. Growth Factor Support
- G-CSF (Granulocyte-Colony Stimulating Factor): Helps manage neutropenia.
4. Targeted Therapy
- JAK-STAT inhibitors: Under investigation for STAT3-mutated cases.
5. Hematopoietic Stem Cell Transplant (HSCT)
- Considered for aggressive, treatment-resistant cases.
Prognosis and Long-Term Outlook
- LGL leukemia has a favorable prognosis, with many patients living decades post-diagnosis.
- Chronic neutropenia and infections are the most common complications.
- Regular monitoring is essential to detect disease progression or secondary malignancies.
Frequently Asked Questions:
1. Is LGL leukemia a type of blood cancer?
Yes, it is a chronic lymphoproliferative disorder that affects lymphocytes.
2. Can LGL leukemia be cured?
There is no definitive cure, but treatment can manage symptoms effectively.
3. How is LGL leukemia different from other leukemias?
Unlike acute leukemias, LGL leukemia progresses slowly and is often associated with autoimmune disorders.
4. Is LGL leukemia hereditary?
No, it is not considered an inherited disease, but genetic mutations play a role in its development.
5. What is the life expectancy of LGL leukemia patients?
Most patients have a normal or near-normal life expectancy with proper management.
Large granular lymphocytic leukemia is a rare but manageable chronic hematologic disorder. Early diagnosis and appropriate treatment strategies can significantly improve the quality of life for affected individuals. Ongoing research into targeted therapies continues to offer hope for better outcomes in the future.

