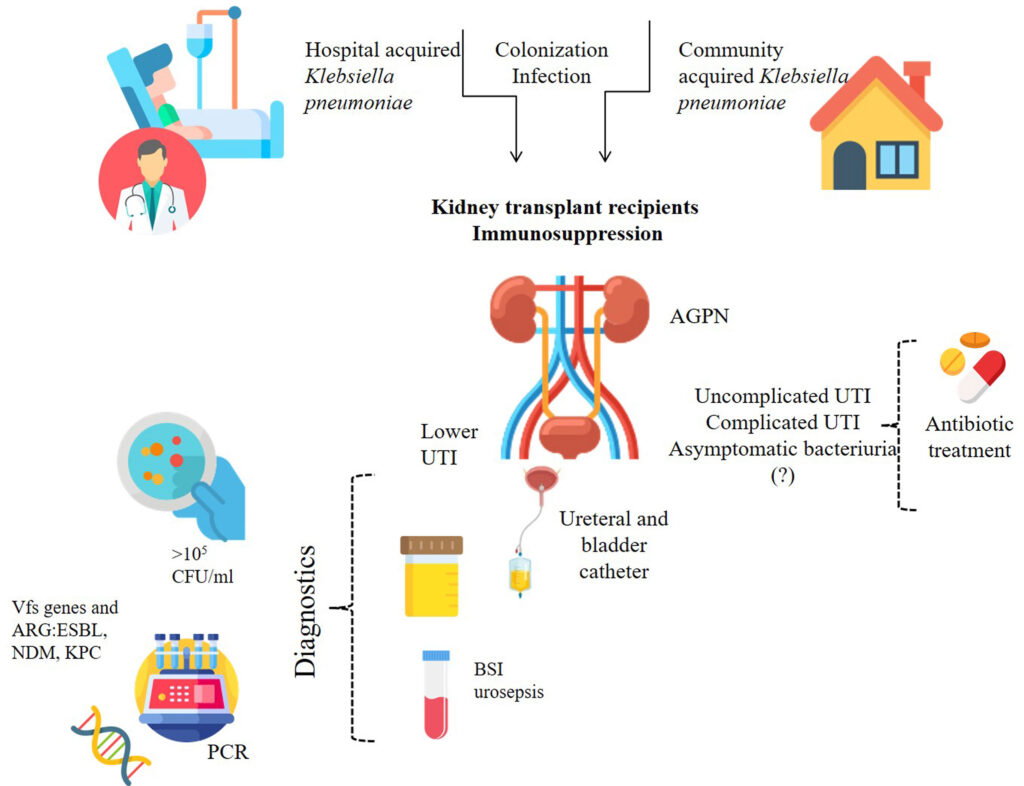
Klebsiella urinary tract infection (UTI) is caused by Klebsiella pneumoniae, a Gram-negative bacterium commonly found in the human gut. While generally harmless in the intestines, it can cause severe infections when it enters the urinary tract, especially in individuals with weakened immune systems or those with urinary catheters.
Causes and Risk Factors
Klebsiella UTIs typically occur due to:
- Hospitalization: Patients in healthcare settings, particularly those with catheters or prolonged antibiotic use, are at higher risk.
- Immunocompromised Conditions: Diabetes, cancer, and organ transplants increase susceptibility.
- Poor Hygiene Practices: Improper handwashing and inadequate personal hygiene can contribute to infection.
- Recent Antibiotic Use: Prior antibiotic treatment can disrupt normal bacterial balance, favoring Klebsiella overgrowth.
- Urinary Tract Abnormalities: Conditions such as kidney stones or structural defects can facilitate bacterial colonization.
Symptoms of Klebsiella UTI
Symptoms of a Klebsiella-induced UTI can range from mild to severe and include:
- Frequent and painful urination (dysuria)
- Cloudy or foul-smelling urine
- Blood in the urine (hematuria)
- Lower abdominal or pelvic pain
- Fever and chills (indicating a more severe infection)
- Fatigue and general discomfort
Diagnosis of Klebsiella UTI
To confirm a Klebsiella UTI, healthcare providers may perform:
- Urinalysis: Detects white blood cells, red blood cells, and bacteria in urine.
- Urine Culture: Identifies Klebsiella pneumoniae and determines antibiotic susceptibility.
- Blood Tests: May be required if the infection has spread to the bloodstream.
- Imaging Tests: Ultrasound or CT scan if structural abnormalities are suspected.
Treatment Options
Treatment varies based on severity and antibiotic resistance patterns.
First-Line Antibiotics
- Trimethoprim-sulfamethoxazole (TMP-SMX)
- Nitrofurantoin
- Fosfomycin
Hospital-Acquired Klebsiella UTI Treatment
- Carbapenems (e.g., meropenem, imipenem) for multidrug-resistant (MDR) strains
- Aminoglycosides (e.g., gentamicin) in combination therapy
- Colistin or tigecycline for extensively drug-resistant (XDR) infections
Antibiotic Resistance Concerns
Klebsiella species are known for producing Extended-Spectrum Beta-Lactamases (ESBLs) and Carbapenem-Resistant Enterobacteriaceae (CRE), making treatment challenging. Proper antibiotic stewardship is essential.
Prevention Strategies
Personal Hygiene and Lifestyle Changes
- Drink plenty of water to flush out bacteria.
- Maintain proper genital hygiene, especially after using the toilet.
- Urinate frequently and avoid holding in urine for prolonged periods.
Hospital and Healthcare Precautions
- Regular catheter care to prevent bacterial colonization.
- Proper hand hygiene by healthcare workers and patients.
- Avoid unnecessary antibiotic use to reduce resistance development.
Complications of Klebsiella UTI
Untreated or severe infections can lead to:
- Pyelonephritis: Infection spreading to the kidneys, causing back pain and high fever.
- Sepsis: A life-threatening response if bacteria enter the bloodstream.
- Chronic UTIs: Recurrent infections requiring long-term management.
Prognosis and Recovery
With prompt treatment, most Klebsiella UTIs resolve within 7 to 14 days. However, complications or antibiotic resistance may prolong recovery.
Klebsiella urinary tract infections are a growing concern, particularly due to antibiotic resistance. Early diagnosis, appropriate treatment, and preventive measures are essential for effective management. If you experience UTI symptoms, seek medical attention promptly.