Klebsiella septicemia, also known as Klebsiella pneumoniae bacteremia, is a life-threatening bloodstream infection caused by the Gram-negative bacillus Klebsiella pneumoniae. This opportunistic pathogen is a major cause of hospital-acquired and multidrug-resistant infections, leading to severe complications such as septic shock and multi-organ failure. Early detection and targeted antibiotic therapy are critical for patient survival.
Pathogenesis and Risk Factors
How Klebsiella Causes Septicemia
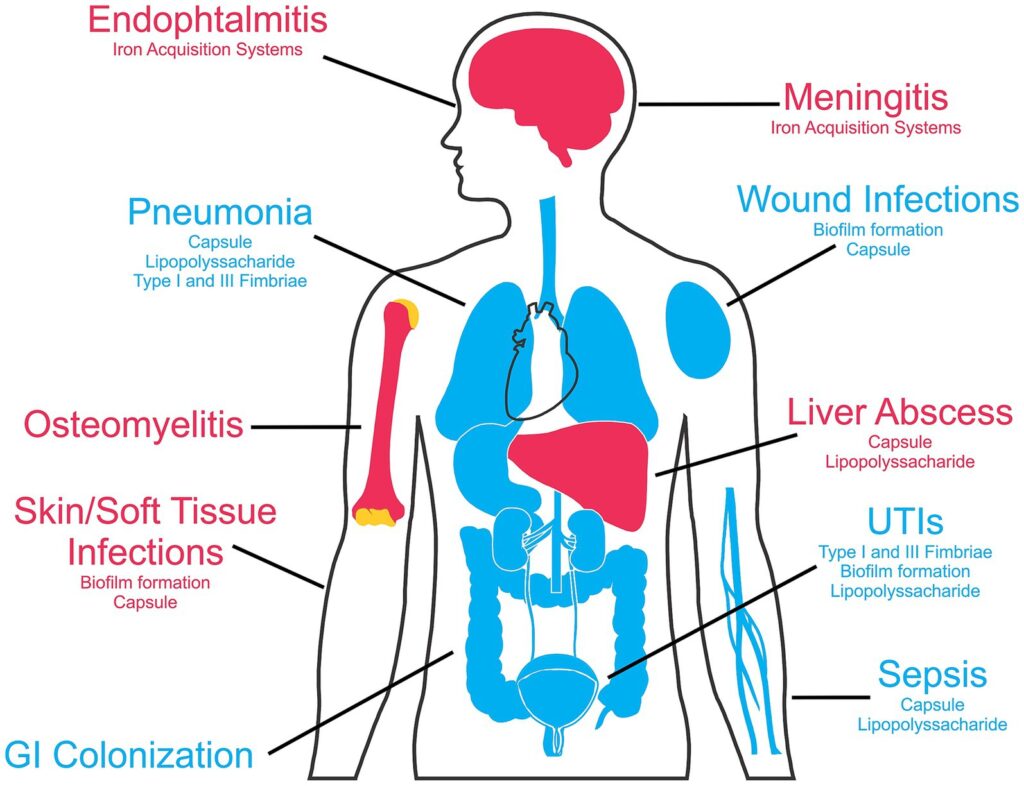
Klebsiella pneumoniae enters the bloodstream through various routes, initiating a systemic inflammatory response. Key mechanisms include:
- Capsular Polysaccharides (K1/K2 Serotypes) – Shields bacteria from phagocytosis.
- Lipopolysaccharide (LPS) – Triggers an excessive immune response, leading to sepsis.
- Fimbriae and Adhesins – Facilitates colonization of epithelial and endothelial surfaces.
- Hypervirulent Strains (hvKP) – Associated with invasive infections, including liver abscesses and meningitis.
- Extended-Spectrum Beta-Lactamase (ESBL) and Carbapenemase Production – Confers resistance to broad-spectrum antibiotics.
Risk Factors for Klebsiella Septicemia
Several conditions predispose individuals to Klebsiella bloodstream infections:
- Hospitalization in Intensive Care Units (ICU) – Increased exposure to invasive procedures.
- Immunocompromised States – Cancer, diabetes, HIV, organ transplantation.
- Prolonged Use of Urinary or Vascular Catheters – Provides direct entry for bacteria.
- Recent Surgery or Trauma – Disrupts natural barriers.
- Long-Term Antibiotic Use – Promotes selection of resistant strains.
- Chronic Respiratory Diseases – Ventilator-associated pneumonia (VAP) increases risk.
Clinical Manifestations
Common Symptoms of Klebsiella Septicemia
- High Fever (>38.5°C / 101.3°F) – A hallmark of systemic infection.
- Chills and Rigors – Indicative of bacteremia.
- Hypotension (Low Blood Pressure) – May progress to septic shock.
- Tachycardia (Rapid Heart Rate) – Compensatory response to sepsis.
- Altered Mental Status – Ranges from confusion to coma in severe cases.
- Respiratory Distress – If pneumonia is the primary source of infection.
- Skin Lesions or Necrosis – In cases of invasive hypervirulent strains.
Complications and Severe Outcomes
- Septic Shock – Life-threatening drop in blood pressure.
- Acute Kidney Injury (AKI) – Due to systemic inflammation and reduced perfusion.
- Multi-Organ Dysfunction Syndrome (MODS) – Failure of vital organs.
- Meningitis and Brain Abscesses – Seen in hypervirulent Klebsiella infections.
Diagnosis of Klebsiella Septicemia
Laboratory Tests
- Blood Cultures – Confirms the presence of Klebsiella pneumoniae in the bloodstream.
- Complete Blood Count (CBC) – Elevated white blood cell count (leukocytosis).
- C-Reactive Protein (CRP) & Procalcitonin – Markers of systemic inflammation.
- Serum Lactate Levels – Indicator of sepsis severity.
- Urinalysis & Sputum Culture – Identifies primary infection source.
Imaging and Advanced Diagnostics
- Chest X-ray or CT Scan – Evaluates lung involvement in pneumonia-associated septicemia.
- Abdominal Ultrasound – Detects liver abscesses in hypervirulent strains.
- Echocardiography – Assesses for endocarditis in high-risk patients.
Treatment Strategies
Empirical and Targeted Antibiotic Therapy
Empirical Treatment (Before Culture Results)
- Mild to Moderate Cases: IV ceftriaxone or piperacillin-tazobactam.
- Severe or ESBL-Producing Strains: Carbapenems (meropenem, imipenem).
- Carbapenem-Resistant Klebsiella (CRKP): Colistin, tigecycline, or fosfomycin-based combination therapy.
Definitive Treatment (Based on Sensitivity Testing)
- Non-Resistant Strains: Third-generation cephalosporins.
- Multidrug-Resistant (MDR) Strains: Aminoglycosides or ceftazidime-avibactam.
- Hypervirulent Strains: Combination therapy with adjunctive drainage of abscesses.
Supportive Care for Septicemia
- Intravenous Fluids (IVF) – Maintains blood pressure and prevents shock.
- Vasopressors (Norepinephrine, Dopamine) – Used in refractory hypotension.
- Oxygen Therapy or Mechanical Ventilation – Required in respiratory failure.
- Renal Replacement Therapy (Dialysis) – If acute kidney injury develops.
Prevention and Infection Control
Hospital-Based Prevention Strategies
- Strict Hand Hygiene Compliance – Reduces transmission risk.
- Aseptic Techniques in Catheter and IV Line Management – Prevents bacterial entry.
- Regular Screening for High-Risk Patients – Identifies colonization early.
- Antibiotic Stewardship Programs – Prevents resistance emergence.
General Preventive Measures
- Proper Wound Care – Minimizes infection risk in post-surgical patients.
- Vaccination Against Pneumococcal and Influenza Infections – Reduces secondary bacterial infections.
- Blood Sugar Control in Diabetic Patients – Lowers susceptibility to infections.
Klebsiella septicemia is a critical medical emergency with high morbidity and mortality rates, especially in immunocompromised and hospitalized patients. The emergence of multidrug-resistant Klebsiella strains complicates treatment, necessitating timely diagnosis and aggressive antimicrobial therapy. Strict infection control measures and antibiotic stewardship are essential in combating this deadly pathogen.