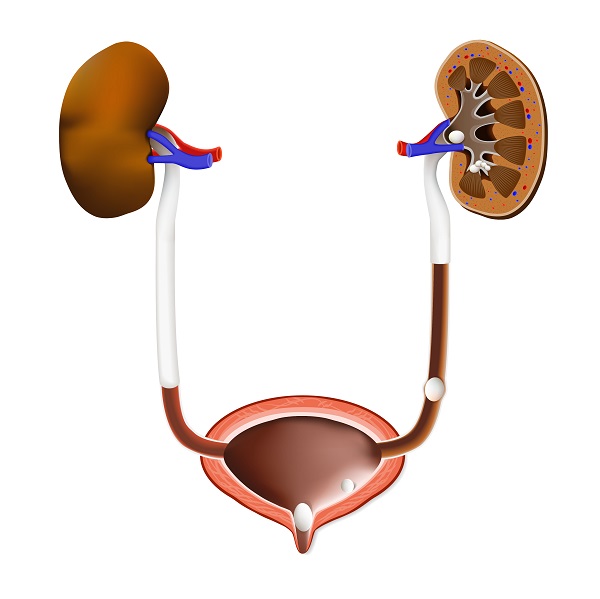
Klebsiella pyelonephritis is a severe bacterial infection of the kidneys caused by Klebsiella pneumoniae, a Gram-negative, facultatively anaerobic bacillus. This pathogen is increasingly recognized in complicated urinary tract infections (UTIs), particularly in hospitalized or immunocompromised patients. Understanding the pathogenesis, clinical presentation, and management of Klebsiella-induced pyelonephritis is crucial for prompt treatment and improved patient outcomes.
Pathogenesis and Risk Factors
Pathogenesis of Klebsiella Pyelonephritis
Klebsiella pneumoniae colonizes the gastrointestinal and urinary tracts and possesses several virulence factors contributing to kidney infections:
- Capsular Polysaccharides (K1, K2 Serotypes) – Protect against host immune responses.
- Fimbriae and Adhesins – Promote bacterial adherence to renal epithelium.
- Biofilm Formation – Enhances resistance to antibiotics and immune clearance.
- Extended-Spectrum Beta-Lactamase (ESBL) Production – Confers resistance to beta-lactam antibiotics.
- Hypervirulent Strains (hvKP) – Capable of causing severe systemic infections.
Risk Factors for Infection
Certain conditions increase susceptibility to Klebsiella pyelonephritis:
- Urinary Catheterization – Prolonged catheter use facilitates bacterial entry.
- Diabetes Mellitus – Impaired immunity increases infection risk.
- Kidney Stones (Nephrolithiasis) – Obstructed urinary flow fosters bacterial growth.
- Immunosuppression – Organ transplant recipients, chemotherapy patients, and those on immunosuppressive therapy are at higher risk.
- Recent Antibiotic Use – Selects for resistant Klebsiella strains.
- Nosocomial Exposure – Hospitalized patients, especially in intensive care units, face a higher likelihood of infection.
Clinical Manifestations
Acute Klebsiella Pyelonephritis
- Fever and Chills – Systemic inflammatory response to bacterial infection.
- Flank Pain – Localized to the affected kidney.
- Dysuria – Painful urination, often accompanied by increased frequency and urgency.
- Nausea and Vomiting – Indicative of systemic involvement.
- Costovertebral Angle Tenderness (CVA Tenderness) – A key diagnostic sign.
- Hematuria (Blood in Urine) – May be present in severe cases.
Complicated Pyelonephritis and Urosepsis
- Severe Sepsis or Septic Shock – Hypotension, multi-organ dysfunction, and altered mental status.
- Renal Abscess Formation – Can lead to kidney damage if untreated.
- Persistent Bacteriuria – Despite antibiotic therapy, indicative of treatment failure or resistance.
Diagnostic Approaches
Laboratory Investigations
- Urinalysis – Pyuria (WBCs in urine), hematuria, and nitrites suggest infection.
- Urine Culture & Sensitivity Testing – Identifies Klebsiella pneumoniae and guides antibiotic selection.
- Blood Cultures – Essential in febrile cases to detect systemic infection.
Imaging Studies
- Renal Ultrasound – Detects hydronephrosis, abscess formation, or anatomical abnormalities.
- CT Scan with Contrast – Preferred in complicated cases to assess renal involvement.
Treatment Strategies
Antibiotic Therapy
Empirical Therapy (Before Culture Results)
- Mild to Moderate Cases: Oral fluoroquinolones (ciprofloxacin, levofloxacin).
- Severe or Complicated Cases: Intravenous ceftriaxone, piperacillin-tazobactam, or carbapenems for ESBL-producing Klebsiella.
Targeted Therapy (Based on Culture Results)
- Non-Resistant Strains: Third-generation cephalosporins (ceftriaxone, cefotaxime).
- ESBL-Producing Strains: Carbapenems (meropenem, imipenem).
- Hypervirulent Klebsiella (hvKP): Combination therapy with aminoglycosides (gentamicin) or colistin may be necessary.
Supportive Care
- Intravenous Fluids – To maintain hydration and renal perfusion.
- Pain Management – NSAIDs or acetaminophen for fever and flank pain.
- Drainage Procedures – Required in cases of renal abscesses or obstruction.
Prevention and Risk Mitigation
General Preventive Measures
- Hydration – Increased fluid intake promotes urine flow, reducing bacterial adherence.
- Good Personal Hygiene – Reduces risk of fecal-urinary transmission.
- Cranberry Extracts – Potentially beneficial in preventing recurrent UTIs.
Hospital Infection Control Measures
- Aseptic Catheterization Practices – Minimizes catheter-associated UTIs.
- Antibiotic Stewardship Programs – Prevents emergence of drug-resistant Klebsiella strains.
- Regular Screening for High-Risk Patients – Early detection in immunocompromised individuals.
Klebsiella pyelonephritis is a serious kidney infection that requires prompt diagnosis and appropriate antibiotic therapy. The rise of multidrug-resistant Klebsiella strains, including ESBL-producing and hypervirulent variants, poses significant treatment challenges. Timely intervention, adherence to preventive measures, and antimicrobial stewardship are critical in reducing morbidity and improving patient outcomes.