Klebsiella pneumoniae is a Gram-negative bacterium that has emerged as a significant pathogen in healthcare settings. Among its various manifestations, septicemia—where the bacteria invade the bloodstream—poses a critical threat due to its rapid progression and high mortality rates. This article provides a detailed exploration of K. pneumoniae septicemia, focusing on its pathogenesis, clinical features, diagnostic approaches, treatment modalities, and preventive measures.
Pathogenesis of Klebsiella pneumoniae Septicemia
The development of septicemia involves several key steps:
- Colonization: K. pneumoniae often colonizes mucosal surfaces, particularly in the respiratory and gastrointestinal tracts.
- Invasion: Breaches in mucosal barriers, due to factors like medical procedures or underlying diseases, allow the bacteria to enter the bloodstream.
- Immune Evasion: The bacterium’s polysaccharide capsule inhibits phagocytosis, facilitating survival in the host.
- Dissemination: Once in the bloodstream, K. pneumoniae can disseminate to various organs, leading to systemic inflammatory responses.
Clinical Manifestations
Septicemia caused by K. pneumoniae presents with:
- Fever and Chills: Sudden onset of high fever accompanied by shaking chills.
- Hypotension: Low blood pressure resulting from systemic vasodilation.
- Tachycardia and Tachypnea: Increased heart and respiratory rates as compensatory mechanisms.
- Altered Mental Status: Confusion or decreased consciousness due to reduced cerebral perfusion.
- Organ Dysfunction: Potential impairment of organs such as kidneys, liver, and lungs, leading to conditions like acute respiratory distress syndrome (ARDS).
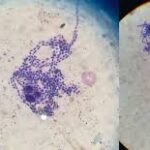
Diagnostic Approaches
Timely and accurate diagnosis is crucial:
- Blood Cultures: Isolation of K. pneumoniae from blood samples confirms septicemia.
- Antibiotic Susceptibility Testing: Determines the resistance profile to guide appropriate therapy.
- Biomarkers: Elevated levels of markers like procalcitonin and C-reactive protein (CRP) indicate systemic inflammation.
Treatment Strategies
Management involves:
- Empirical Antibiotic Therapy: Initiation of broad-spectrum antibiotics covering Gram-negative organisms until specific susceptibilities are known.
- Targeted Antibiotic Therapy: Adjustment based on culture results. For strains producing extended-spectrum beta-lactamases (ESBLs), carbapenems are often required. However, the emergence of carbapenem-resistant K. pneumoniae (CRKP) necessitates the use of agents like colistin or tigecycline.
- Supportive Care: Maintenance of hemodynamic stability through intravenous fluids and vasopressors, along with organ support as needed.
Preventive Measures
Preventing K. pneumoniae septicemia includes:
- Infection Control Practices: Adherence to hand hygiene and sterilization protocols in healthcare settings.
- Antimicrobial Stewardship: Judicious use of antibiotics to minimize the development of resistant strains.
- Surveillance Programs: Monitoring infection rates to identify and control outbreaks promptly.
Klebsiella pneumoniae septicemia represents a formidable challenge in modern medicine, particularly with the rise of hypervirulent and multidrug-resistant strains. A comprehensive approach encompassing prevention, early diagnosis, and effective treatment is essential to improve patient outcomes.