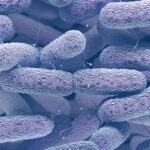
Klebsiella pneumoniae bronchitis is a respiratory condition caused by the opportunistic gram-negative bacterium Klebsiella pneumoniae. This pathogen is known for its resistance to multiple antibiotics and its ability to cause severe infections, particularly in individuals with weakened immune systems. This article explores the causes, symptoms, risk factors, diagnostic methods, and treatment options available for Klebsiella pneumoniae-induced bronchitis.
Understanding Klebsiella pneumoniae and Its Role in Bronchitis
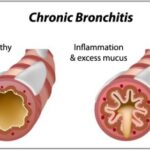
Klebsiella pneumoniae is commonly found in the human gastrointestinal tract but can become pathogenic when it spreads to the respiratory system. It is a major cause of nosocomial infections, particularly in intensive care units (ICUs). When K. pneumoniae infects the bronchial tubes, it can lead to acute or chronic bronchitis, characterized by persistent inflammation and mucus production.
Causes and Risk Factors
Several factors contribute to the development of Klebsiella pneumoniae bronchitis:
- Hospitalization and Ventilator Use: Patients on mechanical ventilation have a higher risk of acquiring K. pneumoniae infections.
- Immunosuppression: Individuals with weakened immune systems, such as those with diabetes, cancer, or HIV, are more susceptible.
- Chronic Respiratory Conditions: Patients with chronic obstructive pulmonary disease (COPD) or cystic fibrosis are at increased risk.
- Antibiotic Use: Prolonged antibiotic treatment can disrupt normal microbiota, promoting K. pneumoniae colonization.
- Aspiration: Inhalation of contaminated secretions can introduce K. pneumoniae into the lungs.
Symptoms of Klebsiella pneumoniae Bronchitis
Symptoms vary depending on the severity of the infection but commonly include:
- Persistent cough with thick, blood-tinged mucus
- Fever and chills
- Shortness of breath
- Chest pain or discomfort
- Fatigue and weakness
- Wheezing and difficulty breathing
In severe cases, K. pneumoniae bronchitis may progress to pneumonia, leading to respiratory failure if left untreated.
Diagnosis of Klebsiella pneumoniae Bronchitis
A comprehensive diagnosis involves multiple laboratory and imaging tests:
- Sputum Culture: Identifies the presence of Klebsiella pneumoniae in respiratory secretions.
- Blood Tests: Elevated white blood cell count (leukocytosis) may indicate infection.
- Chest X-ray or CT Scan: Detects lung inflammation and bronchial abnormalities.
- Polymerase Chain Reaction (PCR): Confirms bacterial DNA in respiratory samples for precise identification.
- Antibiotic Susceptibility Testing: Determines effective antibiotics for treatment.
Treatment Options for Klebsiella pneumoniae Bronchitis
1. Antibiotic Therapy
Treatment is challenging due to K. pneumoniae‘s antibiotic resistance. Empirical therapy may include:
- Carbapenems (e.g., meropenem, imipenem): Effective against multidrug-resistant (MDR) strains.
- Cephalosporins (e.g., cefepime, ceftazidime): Used in less-resistant infections.
- Fluoroquinolones (e.g., levofloxacin): Occasionally effective but resistance is increasing.
- Polymyxins (e.g., colistin): Reserved for carbapenem-resistant infections.
2. Adjunctive Therapies
- Mucolytics and Bronchodilators: Help clear mucus and improve airflow.
- Oxygen Therapy: For patients experiencing respiratory distress.
- Corticosteroids: Reduce bronchial inflammation.
3. Supportive Care
- Hydration to thin mucus
- Pulmonary rehabilitation for chronic cases
- Mechanical ventilation for respiratory failure
Prevention and Infection Control
Prevention strategies focus on reducing transmission, especially in healthcare settings:
- Hand Hygiene: Frequent handwashing with antiseptic solutions.
- Sterile Medical Equipment: Disinfection of ventilators and bronchoscopes.
- Antibiotic Stewardship: Restricting unnecessary antibiotic use to prevent resistance.
- Vaccination: Influenza and pneumococcal vaccines help prevent secondary infections.
Klebsiella pneumoniae bronchitis is a serious respiratory condition requiring prompt diagnosis and targeted antibiotic treatment. Due to its high antibiotic resistance, early intervention and infection control measures are critical in preventing complications.