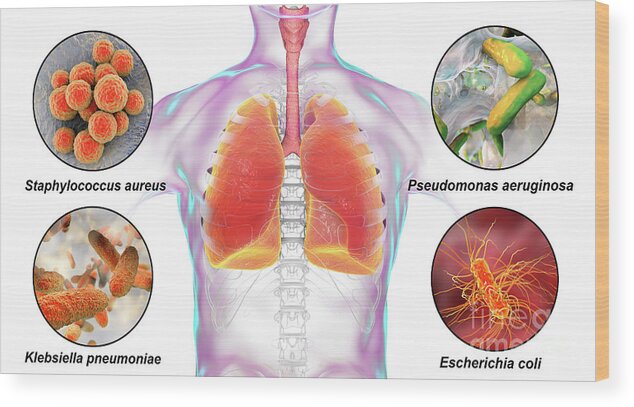
Klebsiella nosocomial pneumonia is a serious hospital-acquired infection caused by Klebsiella pneumoniae, a gram-negative bacterium. It is a leading cause of ventilator-associated pneumonia (VAP) in intensive care units (ICUs) and poses a significant challenge due to its high resistance to antibiotics. This article explores its causes, symptoms, diagnostic methods, treatment options, and preventive measures.
Causes and Risk Factors
Klebsiella pneumoniae is an opportunistic pathogen primarily affecting immunocompromised individuals. The main risk factors include:
- Hospitalization – Especially prolonged stays in ICUs.
- Ventilator Use – Mechanical ventilation increases the risk of infection.
- Weakened Immune System – Patients with chronic illnesses, diabetes, or undergoing chemotherapy are at higher risk.
- Use of Invasive Devices – Such as catheters and endotracheal tubes.
- Antibiotic Use – Prior exposure to broad-spectrum antibiotics may lead to multidrug-resistant Klebsiella infections.
Symptoms of Klebsiella Nosocomial Pneumonia
Symptoms of Klebsiella pneumonia can vary in severity but typically include:
- High fever and chills
- Productive cough with thick, blood-tinged sputum (currant jelly sputum)
- Chest pain and shortness of breath
- Fatigue and confusion (especially in elderly patients)
- Increased respiratory distress in ventilated patients
Diagnosis
1. Clinical Examination
A thorough assessment of symptoms and medical history is crucial, especially in hospitalized patients.
2. Microbiological Testing
- Sputum Culture – Confirms the presence of Klebsiella pneumoniae.
- Bronchoalveolar Lavage (BAL) – Used for intubated patients to obtain deep lung samples.
- Blood Culture – Identifies bacteremia in severe cases.
3. Imaging Techniques
- Chest X-ray – Shows lobar pneumonia with consolidation.
- CT Scan – Detects lung abscesses and cavitation.
4. Antibiotic Susceptibility Testing
Identifies drug-resistant strains to guide appropriate antibiotic therapy.
Treatment Options
1. Antibiotic Therapy
The choice of antibiotics depends on resistance patterns. Common options include:
- Carbapenems – Effective against Extended-Spectrum Beta-Lactamase (ESBL)-producing Klebsiella.
- Polymyxins (Colistin, Polymyxin B) – Used for carbapenem-resistant strains.
- Cephalosporins + Beta-Lactamase Inhibitors – Alternative treatment for susceptible strains.
- Aminoglycosides (Gentamicin, Amikacin) – Often used in combination therapy.
2. Supportive Care
- Oxygen therapy or mechanical ventilation for respiratory distress.
- Fluid management to prevent sepsis-related complications.
- Monitoring for multi-organ failure in severe cases.
Prevention Strategies
1. Infection Control Measures
- Hand Hygiene – Regular handwashing and use of alcohol-based sanitizers.
- Contact Precautions – Isolation of infected patients to prevent transmission.
- Disinfection of Equipment – Regular sterilization of ventilators and invasive devices.
2. Antibiotic Stewardship
- Restricting unnecessary antibiotic use to prevent resistance development.
- Implementing de-escalation strategies based on culture reports.
3. Vaccination and Prophylaxis
- Development of vaccines targeting Klebsiella pneumoniae is underway.
- Use of probiotics and immune-boosting therapies in high-risk patients.
Epidemiology and Global Impact
Klebsiella pneumoniae nosocomial infections are rising globally, particularly in healthcare settings with high antibiotic use. The emergence of multidrug-resistant (MDR) strains has led to outbreaks, emphasizing the need for stringent infection control measures.
Klebsiella nosocomial pneumonia remains a major public health concern due to its high mortality rate and antibiotic resistance. Early detection, prompt antibiotic therapy, and rigorous infection control strategies are crucial in managing and preventing this severe hospital-acquired infection.

