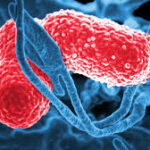
Klebsiella joint infections, also known as Klebsiella-induced septic arthritis, are rare but severe bacterial infections affecting natural and prosthetic joints. Klebsiella pneumoniae and other species in the Klebsiella genus can invade joint spaces, leading to inflammation, cartilage destruction, and functional impairment. These infections are more prevalent in immunocompromised individuals, patients with underlying medical conditions, and those who have undergone joint replacement surgery. Given the rise of multidrug-resistant (MDR) Klebsiella strains, prompt diagnosis and aggressive treatment are essential to prevent long-term complications.

Understanding Klebsiella Joint Infection
Klebsiella species are gram-negative, encapsulated bacteria that normally reside in the human gastrointestinal tract. While they are typically commensal, they can become opportunistic pathogens, causing severe infections when they enter sterile body sites, such as joints. Klebsiella joint infections often result from hematogenous spread (via the bloodstream) or direct inoculation during surgical procedures, trauma, or invasive medical interventions.
Causes and Risk Factors
1. Modes of Transmission
- Hematogenous spread: Bacteria enter the bloodstream from a distant infection, such as pneumonia or urinary tract infections (UTIs), and seed into the joint.
- Direct inoculation: Contamination during joint surgery, intra-articular injections, or penetrating injuries.
- Contiguous spread: Infection spreads from adjacent tissues, such as osteomyelitis or soft tissue infections.
2. Risk Factors
- Prosthetic joint replacement (hip or knee arthroplasty)
- Diabetes mellitus and chronic kidney disease
- Immunosuppression (chemotherapy, organ transplantation, HIV/AIDS)
- Rheumatoid arthritis or other inflammatory joint diseases
- Intravenous drug use
- Recent hospitalization or prolonged use of invasive devices
Clinical Presentation and Symptoms
Klebsiella joint infections present with acute or subacute symptoms, often mimicking inflammatory arthritis. The hallmark signs include:
- Severe joint pain (commonly affecting the knee, hip, or shoulder)
- Joint swelling and warmth
- Restricted range of motion and stiffness
- Fever and chills
- Erythema (redness) over the affected joint
In prosthetic joint infections (PJIs), symptoms may be more insidious, with chronic pain, instability, and mild inflammation rather than acute swelling and fever.
Diagnosis of Klebsiella Joint Infection
1. Laboratory Tests
- Blood cultures: Detect systemic bacteremia, particularly in hematogenous infections.
- Synovial fluid analysis:
- Gram stain and culture: Confirm bacterial presence.
- White blood cell (WBC) count: Typically >50,000 cells/µL in septic arthritis.
- Elevated C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR): Indicate systemic inflammation.
2. Imaging Studies
- X-ray: May show joint effusion but is limited in early infection.
- Ultrasound: Detects fluid accumulation for guided aspiration.
- MRI or CT scan: Helps evaluate bone involvement or deep-seated infections.
Treatment of Klebsiella Joint Infection
1. Antibiotic Therapy
Prompt and targeted antibiotic treatment is crucial, guided by culture and sensitivity results:
- Empirical therapy:
- Third-generation cephalosporins (e.g., ceftriaxone)
- Carbapenems for multidrug-resistant (MDR) Klebsiella strains
- Definitive therapy:
- Based on susceptibility testing, may include aminoglycosides, fluoroquinolones, or tigecycline.
- Duration: 4-6 weeks of intravenous (IV) antibiotics, followed by oral therapy if required.
2. Joint Drainage and Surgical Management
- Arthrocentesis (needle aspiration): Reduces bacterial load in native joint infections.
- Arthroscopic lavage: Minimally invasive method for extensive joint washout.
- Open surgical debridement: Necessary for severe infections or cases involving prosthetic joints.
- Two-stage revision arthroplasty: Required for persistent or chronic prosthetic joint infections.
3. Supportive Care
- Pain management with nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids.
- Physical therapy post-treatment to restore joint mobility.
Antibiotic Resistance in Klebsiella Joint Infections
Klebsiella species have developed resistance to multiple antibiotics, complicating treatment strategies. Key resistance mechanisms include:
- Extended-Spectrum Beta-Lactamases (ESBLs): Confer resistance to penicillins and cephalosporins.
- Carbapenemase production (KPC, NDM, OXA-48): Renders carbapenems ineffective.
- Efflux pumps and biofilm formation: Enhance bacterial survival in prosthetic joints.
Strategies to Combat Resistance
- Combination antibiotic therapy to prevent resistance emergence.
- Rapid molecular diagnostics for early detection of resistant strains.
- Infection control measures to reduce nosocomial transmission.
Prevention of Klebsiella Joint Infections
1. Hospital and Surgical Protocols
- Strict hand hygiene and aseptic techniques during joint procedures.
- Preoperative antibiotic prophylaxis for joint replacement surgeries.
- Enhanced disinfection of surgical instruments and hospital surfaces.
2. Risk Reduction in High-Risk Patients
- Optimizing glycemic control in diabetic patients.
- Avoiding unnecessary invasive procedures or prolonged catheterization.
- Vaccination research targeting Klebsiella pneumoniae to prevent systemic infections.
Klebsiella joint infections, though uncommon, pose significant challenges due to their potential for rapid joint destruction and antibiotic resistance. Early diagnosis through laboratory and imaging studies, coupled with prompt antibiotic therapy and surgical intervention when necessary, is critical to improving outcomes. Preventive measures, including strict infection control practices and judicious use of antibiotics, remain essential in reducing the incidence of these infections. Ongoing research into novel antimicrobial therapies and vaccine development offers hope for better management and prevention of Klebsiella-related orthopedic infections.