Klebsiella infections are a growing global concern due to their increasing antibiotic resistance. Klebsiella pneumoniae, the most common species in this genus, is responsible for severe infections, including pneumonia, urinary tract infections (UTIs), bloodstream infections (sepsis), and soft tissue infections. It is a leading cause of hospital-acquired infections (HAIs) and is particularly dangerous for immunocompromised individuals. Understanding its transmission, symptoms, and treatment options is crucial in managing and preventing outbreaks.

What is Klebsiella Infection?
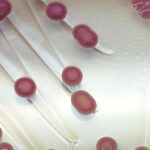
Klebsiella is a gram-negative, rod-shaped bacterium found in the human intestinal tract, soil, and water. While it is usually harmless in healthy individuals, it can become opportunistic, causing severe infections when it spreads beyond the gut. The emergence of multidrug-resistant (MDR) Klebsiella strains, including extended-spectrum beta-lactamase (ESBL) and carbapenem-resistant Klebsiella pneumoniae (CRKP), has made treatment more challenging.
Causes and Risk Factors
1. Transmission and Routes of Infection
- Hospital environments: Contaminated medical equipment, catheters, ventilators, and healthcare personnel can transmit Klebsiella.
- Person-to-person contact: Direct contact with infected individuals, especially in healthcare settings, increases risk.
- Contaminated food and water: Ingestion of bacteria from unclean sources can lead to gastrointestinal infections.
- Aspiration of secretions: Inhaling contaminated respiratory secretions can cause pneumonia.
2. Risk Factors for Severe Infection
- Hospitalization and ICU stay
- Prolonged use of ventilators or catheters
- Diabetes and chronic diseases
- Weakened immune system (HIV/AIDS, chemotherapy, organ transplant recipients)
- Elderly individuals and newborns
Common Types of Klebsiella Infections
1. Klebsiella Pneumonia
- A severe form of bacterial pneumonia, often presenting with fever, chest pain, cough, and bloody sputum (“currant jelly” sputum).
- Common in ventilated patients and those with chronic lung disease.
2. Urinary Tract Infections (UTIs)
- Occurs in catheterized patients or individuals with diabetes.
- Symptoms include frequent urination, burning sensation, fever, and lower abdominal pain.
3. Bloodstream Infections (Sepsis)
- Life-threatening condition when bacteria enter the bloodstream.
- Symptoms include high fever, chills, rapid heartbeat, and organ dysfunction.
4. Soft Tissue and Wound Infections
- Often affects surgical wounds and diabetic foot ulcers.
- Leads to redness, swelling, pus formation, and tissue necrosis.
5. Meningitis
- Rare but severe, occurring in newborns and immunocompromised individuals.
- Symptoms include fever, neck stiffness, seizures, and altered consciousness.
Diagnosis of Klebsiella Infection
1. Laboratory Tests
- Blood cultures: Identify bacterial presence in sepsis cases.
- Sputum cultures: Diagnose pneumonia.
- Urine cultures: Confirm UTIs caused by Klebsiella.
- Wound swabs: Detect skin and soft tissue infections.
2. Imaging Studies
- Chest X-ray or CT scan: Identify lung infections.
- Ultrasound or MRI: Assess deep-seated infections or abscesses.
Treatment of Klebsiella Infections
1. Antibiotic Therapy
Treatment depends on antibiotic susceptibility tests:
- Mild to moderate infections:
- Third-generation cephalosporins (e.g., ceftriaxone)
- Fluoroquinolones (e.g., ciprofloxacin)
- Multidrug-resistant (MDR) infections:
- Carbapenems (e.g., meropenem, imipenem)
- Polymyxins (colistin) in extreme cases
- Severe or hospital-acquired infections:
- Combination therapy with aminoglycosides (amikacin) or tigecycline
2. Supportive Care
- Oxygen therapy and ventilation for pneumonia patients.
- Intravenous fluids and vasopressors for sepsis management.
- Surgical drainage of abscesses if necessary.
Antibiotic Resistance in Klebsiella Infections
Klebsiella species have developed resistance mechanisms, including:
- Extended-Spectrum Beta-Lactamases (ESBLs): Enzymes that break down penicillins and cephalosporins.
- Carbapenem-Resistant Klebsiella pneumoniae (CRKP): Resistant to most beta-lactam antibiotics, requiring last-resort drugs like colistin.
- Efflux pumps and biofilm formation: Reduce antibiotic penetration and enhance bacterial survival.
Strategies to Combat Resistance
- Antibiotic stewardship programs to reduce overuse.
- Rapid diagnostics to tailor antibiotic therapy.
- Infection control measures in healthcare settings.
Prevention Strategies
1. Hospital Infection Control
- Regular disinfection of medical equipment.
- Hand hygiene and personal protective equipment (PPE) use.
- Isolation of infected patients to prevent spread.
2. Vaccination Research
- Efforts are ongoing to develop vaccines targeting Klebsiella pneumoniae.
3. Public Health Measures
- Proper wound care and hygiene.
- Avoiding unnecessary antibiotic use.
Klebsiella infections pose a significant public health challenge due to their ability to cause severe disease and their increasing resistance to antibiotics. Early diagnosis, appropriate antibiotic therapy, and strict infection control measures are essential to managing and preventing these infections. Research into novel treatments, vaccines, and antibiotic stewardship programs is critical in combating this evolving threat.