Endometritis is an inflammatory condition of the endometrial lining of the uterus, often caused by bacterial infections. While Escherichia coli and Staphylococcus species are common culprits, Klebsiella pneumoniae has emerged as a significant pathogen, particularly in hospital-acquired infections and postpartum cases. Given its potential for antibiotic resistance, Klebsiella infections require timely and targeted treatment to prevent complications such as infertility, sepsis, and chronic pelvic inflammatory disease (PID).
Understanding Klebsiella Endometritis
Klebsiella endometritis occurs when Klebsiella bacteria infect the endometrial lining, leading to inflammation, pain, and systemic symptoms. This condition is most frequently observed in postpartum women, post-surgical patients, and individuals with compromised immune systems. If untreated, the infection can spread to surrounding pelvic structures, resulting in severe complications.
Causes and Risk Factors
1. Routes of Infection
- Ascending infection: Bacteria enter the uterus from the lower genital tract, especially after childbirth or gynecological procedures.
- Hematogenous spread: Klebsiella can enter the bloodstream from another site of infection, such as a urinary tract infection (UTI) or pneumonia, and infect the endometrium.
2. Risk Factors
- Postpartum complications: Prolonged labor, cesarean section, or retained placental tissue increase susceptibility.
- Gynecological procedures: Endometrial biopsies, intrauterine device (IUD) insertions, or dilation and curettage (D&C) procedures can introduce bacteria.
- Hospital-acquired infections: Klebsiella is a leading cause of nosocomial infections, especially in post-surgical settings.
- Weakened immunity: Diabetes, HIV, or immunosuppressive therapy raises the risk of severe infection.
- Recurrent UTIs: As Klebsiella frequently causes urinary infections, untreated UTIs can lead to endometrial involvement.
Symptoms of Klebsiella Endometritis
Common Symptoms
- Lower abdominal pain and cramping
- Fever and chills
- Foul-smelling vaginal discharge
- Abnormal uterine bleeding
- Pelvic tenderness
Severe Symptoms Indicating Complications
- High-grade fever and sepsis (suggesting systemic spread)
- Nausea and vomiting (indicating peritoneal involvement)
- Chronic pelvic pain (suggesting untreated or recurrent infection)
Diagnosis of Klebsiella Endometritis
1. Laboratory Tests
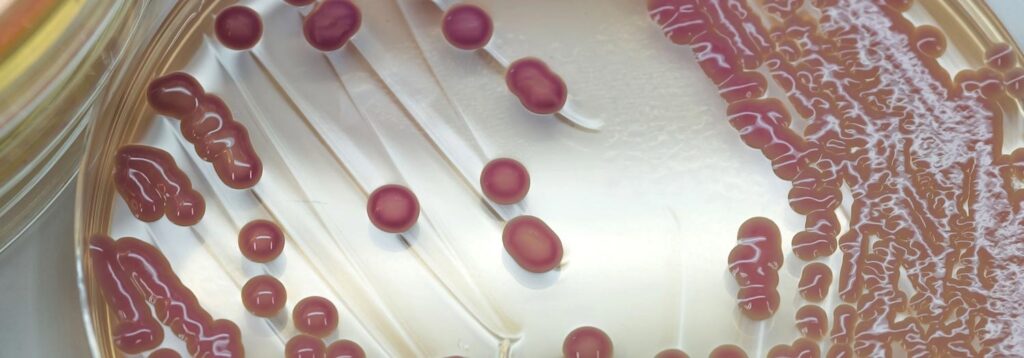
- Endometrial cultures: Confirm Klebsiella presence and determine antibiotic resistance.
- Blood tests: Elevated white blood cell count (WBC) and C-reactive protein (CRP) suggest infection.
- Urinalysis: Checks for concurrent UTIs, which are common in Klebsiella infections.
2. Imaging Studies
- Pelvic ultrasound: Identifies endometrial thickening, abscesses, or retained products of conception.
- MRI or CT scan: Used for severe cases to assess pelvic organ involvement.
Treatment of Klebsiella Endometritis
1. Antibiotic Therapy
Treatment is based on bacterial culture and sensitivity tests:
- Mild to moderate cases:
- Ceftriaxone or cefotaxime (if susceptible)
- Fluoroquinolones (e.g., levofloxacin)
- Severe or resistant infections (ESBL-producing Klebsiella):
- Carbapenems (e.g., meropenem, imipenem)
- Aminoglycosides (e.g., amikacin) in combination therapy
- Postpartum or surgical cases:
- Combination therapy with clindamycin and gentamicin is commonly used.
2. Surgical Interventions (For Complications)
- Dilation and curettage (D&C): Removes infected tissue or retained placenta.
- Drainage of abscesses: In cases of pelvic abscess formation.
Prevention Strategies
- Aseptic Techniques in Hospitals: Ensuring sterile conditions during childbirth and gynecological procedures.
- Proper Postpartum Care: Monitoring for early signs of infection in high-risk patients.
- Antibiotic Stewardship: Preventing the emergence of resistant Klebsiella strains through appropriate antibiotic use.
- Hygiene and Infection Control: Maintaining personal and hospital hygiene to reduce bacterial transmission.
Klebsiella endometritis is a serious bacterial infection requiring early diagnosis and targeted antibiotic therapy to prevent complications. Women undergoing childbirth, surgery, or gynecological procedures should be vigilant for symptoms, while healthcare facilities must implement strict infection control measures to reduce Klebsiella transmission.