Cystitis, a bacterial infection of the bladder, is commonly caused by Escherichia coli but can also result from Klebsiella pneumoniae or Klebsiella oxytoca. Klebsiella species are Gram-negative bacteria known for their antibiotic resistance, particularly in hospital-acquired infections. When Klebsiella causes cystitis, it often presents as a complicated urinary tract infection (UTI), requiring targeted treatment to prevent recurrence and complications.
What is Klebsiella Cystitis?
Klebsiella cystitis occurs when Klebsiella bacteria colonize the bladder, leading to inflammation, pain, and urinary symptoms. While uncomplicated cases may resolve with antibiotics, drug-resistant strains can cause persistent infections, increasing the risk of pyelonephritis (kidney infection) or urosepsis.
Causes and Risk Factors
1. Bacterial Transmission and Colonization
- Klebsiella can enter the urinary tract through poor hygiene, catheterization, or hospital exposure.
- The bacteria adhere to the bladder lining and form biofilms, making eradication difficult.
2. Risk Factors for Klebsiella Cystitis
- Hospital-acquired infections: Long-term catheterization increases risk.
- Antibiotic resistance: ESBL-producing Klebsiella limits treatment options.
- Weakened immunity: Diabetes, chronic kidney disease, and immunosuppressive therapy increase susceptibility.
- Recurrent UTIs: Patients with a history of frequent UTIs are at greater risk.
Symptoms of Klebsiella Cystitis
Common Symptoms
- Dysuria (burning sensation during urination)
- Increased urinary urgency and frequency
- Hematuria (blood in urine)
- Foul-smelling or cloudy urine
- Suprapubic pain or discomfort
Severe Symptoms Indicating Complications
- Fever and chills (suggesting systemic infection)
- Flank pain and nausea (indicating kidney involvement)
- Confusion or delirium in elderly patients
Diagnosis of Klebsiella Cystitis
1. Laboratory Tests
- Urinalysis: Detects leukocytes, nitrites, and bacteria.
- Urine Culture: Identifies Klebsiella species and determines antibiotic susceptibility.
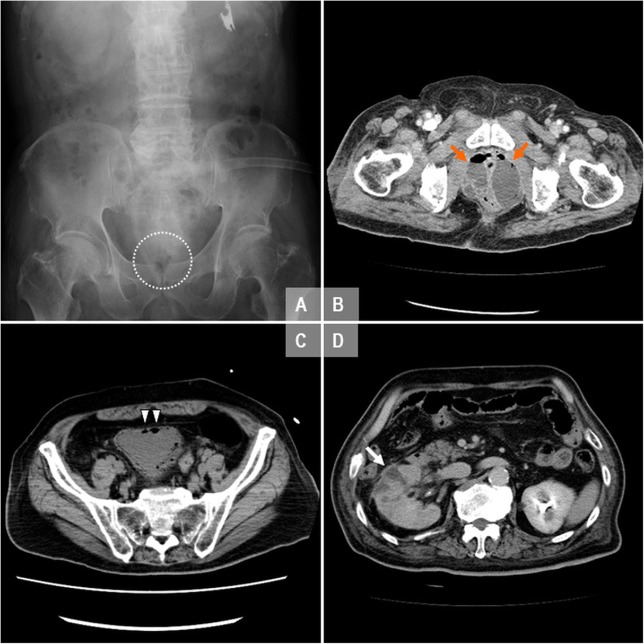
2. Imaging Studies
- Ultrasound or CT scan: Detects structural abnormalities in patients with recurrent infections.
3. Blood Tests (For Severe Cases)
- Complete blood count (CBC): Assesses infection severity.
- C-reactive protein (CRP): Indicates inflammation.
Treatment of Klebsiella Cystitis
1. Antibiotic Therapy
Antibiotic choice depends on culture sensitivity tests:
- First-line treatment:
- Nitrofurantoin or Fosfomycin for non-resistant strains
- Fluoroquinolones (e.g., ciprofloxacin) if effective
- Resistant infections (ESBL-producing Klebsiella):
- Carbapenems (meropenem, imipenem)
- Ceftazidime-avibactam as an alternative
- Recurrent infections:
- Low-dose prophylactic antibiotics in high-risk patients
2. Supportive Care
- Hydration: Flushes bacteria from the bladder.
- Urinary analgesics (phenazopyridine): Relieves discomfort.
Prevention Strategies
- Catheter Care: Reduce prolonged use to prevent hospital-acquired infections.
- Hygiene Practices: Proper wiping techniques and hand hygiene.
- Urinary Health: Staying hydrated and urinating frequently.
- Routine Screening: For patients with recurrent infections or high-risk conditions.
Klebsiella cystitis requires prompt diagnosis and targeted antibiotic therapy due to its potential for drug resistance and severe complications. Preventative measures, including proper catheter management and hygiene, play a crucial role in reducing infection rates. Patients experiencing recurrent infections should undergo further evaluation to prevent long-term damage.