Urinary tract infections (UTIs) are among the most common bacterial infections, but when caused by Klebsiella species, they can become complicated and difficult to treat. Klebsiella pneumoniae and Klebsiella oxytoca are Gram-negative bacteria capable of causing severe UTIs, particularly in immunocompromised individuals or those with underlying conditions. These infections often exhibit antibiotic resistance, making treatment more challenging.
Understanding Klebsiella-Associated Complicated UTIs
A complicated UTI occurs when structural or functional abnormalities of the urinary tract predispose a patient to infection. Klebsiella species, known for their ability to acquire antibiotic resistance, pose a significant threat, especially in hospital-acquired infections.
Unlike uncomplicated UTIs, which typically resolve with standard antibiotics, complicated UTIs caused by Klebsiella may lead to severe complications, including kidney infections (pyelonephritis), sepsis, and urinary retention.
Causes and Risk Factors
1. Bacterial Colonization and Biofilm Formation
- Klebsiella can adhere to the bladder wall and form biofilms, making infections persistent.
- Biofilm-associated infections resist antibiotic penetration, leading to chronic UTIs.
2. Hospital-Acquired Infections
- Catheter-associated UTIs (CAUTIs) are a significant risk factor for Klebsiella infections.
- Prolonged hospitalization and invasive urological procedures increase susceptibility.
3. Antibiotic Resistance and ESBL Production
- Many Klebsiella strains produce extended-spectrum beta-lactamases (ESBLs), rendering common antibiotics ineffective.
- Carbapenem-resistant Klebsiella pneumoniae (CRKP) is an emerging global health concern.
4. Underlying Medical Conditions
- Diabetes mellitus and chronic kidney disease impair immune responses, increasing infection risk.
- Patients with neurogenic bladder dysfunction or urinary tract obstructions are highly vulnerable.
Symptoms of Klebsiella Complicated UTI
Primary Symptoms:
- Dysuria (painful urination)
- Increased urinary frequency and urgency
- Cloudy or foul-smelling urine
- Hematuria (blood in urine)
- Suprapubic or flank pain
Signs of Severe Infection:
- High fever with chills
- Nausea and vomiting
- Lower back pain (suggestive of pyelonephritis)
- Confusion or altered mental status (in elderly patients)
- Septic shock in severe cases
Diagnosis of Klebsiella Complicated UTI
1. Urinalysis and Urine Culture
- Urine dipstick test: Detects leukocytes and nitrites, indicating infection.
- Microscopy: Identifies Gram-negative bacilli.
- Urine culture: Confirms Klebsiella species and determines antibiotic susceptibility.
2. Blood Tests
- Complete blood count (CBC): Elevated white blood cell count suggests systemic infection.
- C-reactive protein (CRP) and procalcitonin: Indicate severe bacterial inflammation.
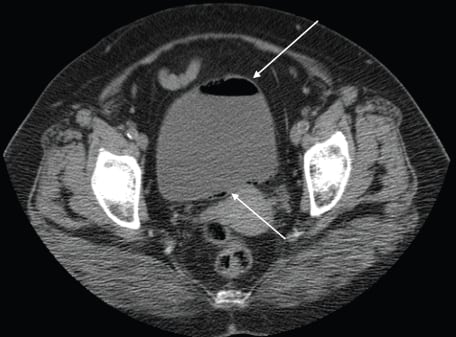
3. Imaging Studies
- Ultrasound: Identifies urinary tract abnormalities such as kidney stones or hydronephrosis.
- CT Scan: Detects abscess formation or complications in recurrent UTIs.
Treatment Strategies for Klebsiella Complicated UTI
1. Targeted Antibiotic Therapy
Given the antibiotic resistance of Klebsiella, empirical treatment should be guided by culture sensitivity results.
- First-line antibiotics:
- Carbapenems (e.g., meropenem, imipenem) for ESBL-producing Klebsiella.
- Fosfomycin or aminoglycosides as alternative agents.
- Second-line options:
- Fluoroquinolones (e.g., ciprofloxacin) if the strain remains susceptible.
- Nitrofurantoin or ceftazidime-avibactam in resistant cases.
2. Management of Recurrent Infections
- Long-term prophylactic antibiotics for high-risk patients.
- Avoidance of unnecessary catheter use and strict catheter care protocols.
3. Hospitalized Patients and Severe Cases
- Intravenous antibiotics for pyelonephritis or urosepsis.
- Hemodynamic support and fluids for septic patients.
- Urological interventions if obstruction or abscess formation is present.
Prevention Strategies
- Strict infection control in healthcare settings to prevent hospital-acquired UTIs.
- Proper catheter management to minimize CAUTI risk.
- Hydration and urinary hygiene to reduce bacterial colonization.
- Regular follow-ups for high-risk patients to detect infections early.
Klebsiella complicated UTIs pose a significant challenge due to their antibiotic resistance and potential for severe complications. Early diagnosis through urine culture and imaging, combined with targeted antibiotic therapy, is essential for successful treatment. Preventive measures, including proper catheter management and infection control, can significantly reduce the risk of recurrent infections.

