Keratoderma refers to a group of disorders characterized by the thickening of the skin’s outer layer, primarily affecting the palms and soles. This condition can be both inherited and acquired, presenting in various forms with differing clinical features.

Classification of Keratoderma
Keratoderma is broadly categorized based on its origin and clinical presentation:
- Inherited (Hereditary) Keratoderma: Resulting from genetic mutations affecting skin proteins like keratin. These can follow autosomal dominant or recessive inheritance patterns.
- Acquired Keratoderma: Developing due to external factors such as underlying medical conditions, infections, medications, or environmental influences.
Clinical Types
- Diffuse Keratoderma: Uniform thickening across the entire palm or sole.
- Focal Keratoderma: Localized thickening, typically over pressure points like heel margins.
- Punctate Keratoderma: Multiple small, discrete areas of thickened skin.
- Striate Keratoderma: Linear thickening extending along the fingers into the palm.
Causes of Keratoderma
Inherited Causes
Hereditary keratodermas arise from genetic mutations affecting keratin production. Notable types include:
- Unna-Thost Type: Autosomal dominant; presents with diffuse thickening from infancy.
- Vorner’s Type: Similar to Unna-Thost but with distinct histological features.
- Mal de Meleda: Autosomal recessive; characterized by diffuse thickening and potential systemic involvement.
Acquired Causes
Acquired keratoderma can result from various factors:
- Inflammatory Skin Conditions: Such as eczema, psoriasis, or lichen planus.
- Infections: Including fungal infections (tinea), syphilis, or scabies.
- Medications and Toxins: Exposure to substances like lithium, arsenic, or certain chemotherapeutic agents.
- Systemic Diseases: Conditions like thyroid disorders, diabetes mellitus, or internal malignancies.
- Circulatory Issues: Chronic lymphoedema can lead to skin thickening.
Symptoms and Clinical Features
Patients with keratoderma may experience:
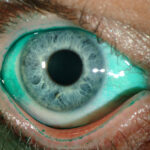
- Thickened, Hard Skin: Often yellowish or red and flaky on palms and soles.
- Pain and Discomfort: Especially when walking or using hands.
- Fissures and Cracks: Leading to potential secondary infections.
- Nail Changes: Thickening or discoloration of nails.
- Excessive Sweating: Particularly on palms and soles.
Diagnosis of Keratoderma
Diagnosis involves:
- Clinical Evaluation: Thorough history and physical examination.
- Genetic Testing: For suspected hereditary cases.
- Laboratory Tests: To identify underlying infections or systemic diseases.
Treatment Options
Treatment aims to manage symptoms and address underlying causes:
Topical Treatments
- Emollients: Moisturizers to soften and hydrate the skin.
- Keratolytic Agents: Such as salicylic acid to exfoliate thickened skin.
- Topical Retinoids: To promote skin cell turnover.
- Topical Corticosteroids: To reduce inflammation.
Systemic Treatments
- Oral Retinoids: Medications like acitretin to reduce skin thickening.
- Treatment of Underlying Conditions: Managing systemic diseases or discontinuing causative medications.
Self-Care Measures
- Regular Foot and Hand Care: Including soaking and filing thickened areas.
- Appropriate Footwear: To reduce pressure on affected areas.
- Managing Sweating: Using moisture-wicking socks or antiperspirants.
Keratoderma encompasses a diverse group of conditions leading to skin thickening on the palms and soles. Understanding its classification, causes, and treatment options is crucial for effective management and improving patient quality of life.