Juvenile Metachromatic Leukodystrophy (MLD) is a rare, inherited neurological disorder that affects the central and peripheral nervous systems. It is characterized by the accumulation of sulfatides due to a deficiency in the enzyme arylsulfatase A (ARSA), leading to progressive demyelination and severe neurological deterioration.
What Is Juvenile Metachromatic Leukodystrophy?
MLD is classified into three main forms: late-infantile, juvenile, and adult-onset. The juvenile form typically manifests between the ages of 4 and 16 and progresses at a slower rate compared to the late-infantile form.
Causes and Genetic Basis
MLD is caused by mutations in the ARSA gene, which provides instructions for producing the arylsulfatase A enzyme. This enzyme is responsible for breaking down sulfatides, a type of fatty substance. In the absence of functional ARSA, sulfatides accumulate in myelin-producing cells, leading to progressive damage and loss of white matter in the brain and nervous system.
Inheritance Pattern
MLD follows an autosomal recessive inheritance pattern, meaning that a child must inherit two defective copies of the ARSA gene (one from each parent) to develop the disease.
Symptoms of Juvenile MLD
Symptoms of juvenile MLD vary but generally include:
- Cognitive Decline: Difficulty with learning, memory loss, and reduced problem-solving skills.
- Motor Dysfunction: Loss of coordination, muscle weakness, and impaired gait.
- Speech and Language Issues: Slurred speech, difficulty in forming sentences, and eventual loss of verbal communication.
- Behavioral Changes: Mood swings, irritability, depression, and social withdrawal.
- Seizures: Some patients may develop epilepsy as the disease progresses.
- Vision and Hearing Loss: Progressive sensory impairments due to demyelination.
Diagnosis
Diagnosing MLD involves a combination of clinical evaluation, biochemical testing, and genetic analysis.
1. Enzyme Assay for ARSA Activity
A laboratory test measures ARSA enzyme activity in leukocytes (white blood cells) to determine deficiency.
2. Urinary Sulfatide Analysis
Elevated levels of sulfatides in urine can indicate MLD.
3. Genetic Testing
DNA sequencing of the ARSA gene confirms mutations associated with MLD.
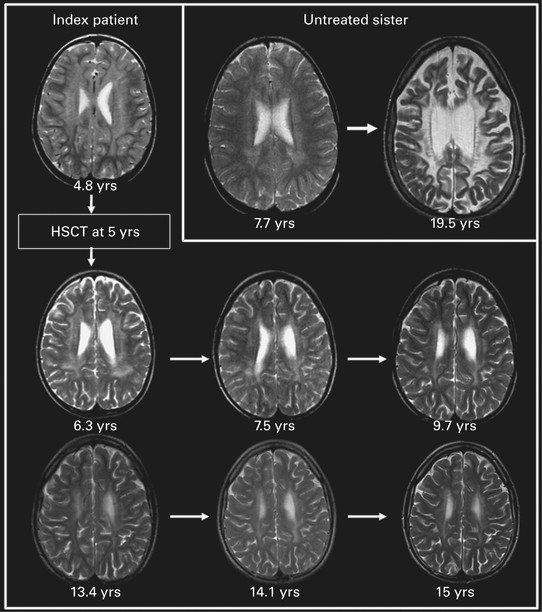
4. MRI Brain Scans
Magnetic Resonance Imaging (MRI) can reveal characteristic white matter abnormalities and demyelination patterns.
5. Nerve Conduction Studies
These tests assess peripheral nerve function and can detect early damage.
Treatment Options
Currently, no cure exists for MLD, but treatment strategies focus on symptom management and slowing disease progression.
1. Hematopoietic Stem Cell Transplantation (HSCT)
- The only potential disease-modifying treatment.
- Works best if performed before symptom onset.
- Uses bone marrow or umbilical cord blood stem cells to restore ARSA enzyme activity.
2. Gene Therapy
- Experimental approaches involve delivering a functional ARSA gene using viral vectors.
- Early trials show promise in slowing disease progression.
3. Supportive and Palliative Care
- Physical Therapy: Helps maintain mobility and prevent contractures.
- Speech and Occupational Therapy: Assists in communication and daily activities.
- Seizure Management: Antiepileptic drugs can help control seizures.
- Nutritional Support: Feeding tubes may be required in later stages.
Prognosis and Life Expectancy
The prognosis for juvenile MLD varies. Without treatment, life expectancy is typically reduced, with severe disability occurring within a decade of symptom onset. However, early intervention with HSCT or emerging gene therapies may improve outcomes.
Prevention and Genetic Counseling
Since MLD is an inherited disorder, genetic counseling is recommended for at-risk families. Carrier screening and prenatal testing can help prospective parents make informed decisions.
Juvenile Metachromatic Leukodystrophy is a devastating genetic disorder that requires early diagnosis and intervention. While no cure exists, ongoing research in gene therapy and stem cell transplantation offers hope for affected individuals. If your family has a history of MLD, genetic counseling and early screening are crucial for informed decision-making.