Invasive bladder cancer is an advanced form of bladder cancer that has spread beyond the inner lining of the bladder into the muscle wall or beyond. It requires prompt diagnosis and aggressive treatment to prevent metastasis and improve survival rates.
Understanding Invasive Bladder Cancer
Bladder cancer originates in the urothelial cells lining the bladder. When the cancer spreads into the muscular layer of the bladder, it is classified as muscle-invasive bladder cancer (MIBC). This progression increases the risk of cancer spreading to nearby organs, lymph nodes, or distant sites.
Causes and Risk Factors
Several factors contribute to the development of invasive bladder cancer:
- Smoking: The leading risk factor, responsible for nearly half of all bladder cancer cases.
- Chemical Exposure: Industrial chemicals such as benzidine and aromatic amines increase risk.
- Chronic Bladder Inflammation: Recurrent urinary infections, bladder stones, or schistosomiasis may contribute.
- Age and Gender: More common in older adults and males.
- Genetic Predisposition: Family history of bladder cancer may increase susceptibility.
Symptoms of Invasive Bladder Cancer
Patients with invasive bladder cancer may experience:
- Hematuria (blood in urine): Most common symptom, often painless.
- Frequent Urination: Urgency or discomfort while urinating.
- Pelvic Pain: Occurs as the cancer invades surrounding tissues.
- Weight Loss and Fatigue: Indicators of advanced disease.
- Lower Back Pain: Suggestive of cancer spreading beyond the bladder.
Diagnosis and Staging
Diagnostic Procedures
To confirm invasive bladder cancer, the following tests are conducted:
- Urinalysis and Urine Cytology: Detects abnormal cancerous cells.
- Cystoscopy: A thin, flexible tube with a camera inspects the bladder lining.
- Biopsy (Transurethral Resection of Bladder Tumor – TURBT): Tissue sample analysis determines cancer stage.
- Imaging Studies: CT scan, MRI, or PET scan to assess tumor invasion and metastasis.
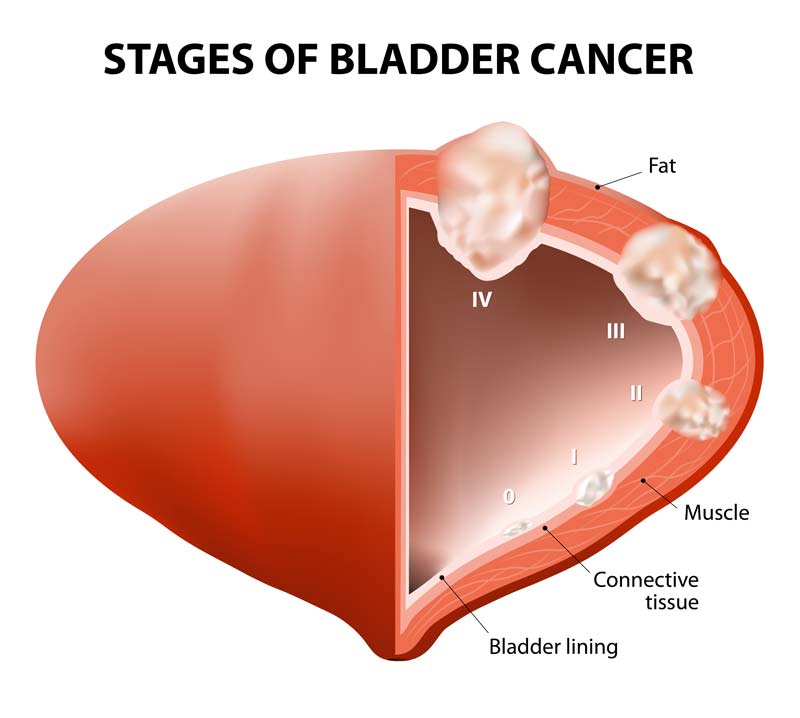
Staging of Invasive Bladder Cancer
Bladder cancer is staged using the TNM (Tumor, Node, Metastasis) system:
- Stage II and beyond indicate muscle invasion, requiring aggressive treatment.
Treatment Options for Invasive Bladder Cancer
1. Surgery
- Radical Cystectomy: Complete removal of the bladder, nearby lymph nodes, and surrounding organs if necessary.
- Urinary Diversion: Neobladder reconstruction or urostomy to restore urine flow.
2. Chemotherapy
- Neoadjuvant Chemotherapy: Administered before surgery to shrink tumors.
- Adjuvant Chemotherapy: Given post-surgery to eliminate remaining cancer cells.
3. Radiation Therapy
- Often combined with chemotherapy for patients unable to undergo surgery.
- Used in bladder-preserving approaches.
4. Immunotherapy and Targeted Therapy
- Checkpoint Inhibitors (e.g., Atezolizumab, Pembrolizumab): Boost the immune system to attack cancer cells.
- FGFR Inhibitors: Target specific genetic mutations in bladder cancer.
5. Bladder-Preserving Therapy
For select patients, a combination of TURBT, chemotherapy, and radiation therapy allows bladder preservation while effectively treating cancer.
Prognosis and Survival Rates
The prognosis of invasive bladder cancer depends on the stage at diagnosis and treatment approach:
- Stage II (Muscle-invasive, no spread): 5-year survival rate ~60%.
- Stage III (Local spread): 5-year survival rate ~40%.
- Stage IV (Metastatic): 5-year survival rate ~5-15%.
Early detection and multimodal treatment significantly improve outcomes.
Invasive bladder cancer is a serious condition requiring timely diagnosis and aggressive treatment. Advances in surgical techniques, chemotherapy, and immunotherapy continue to improve survival rates and patient quality of life. Consultation with a specialized oncologist is crucial for optimal treatment planning.