Gastrointestinal (GI) tract intubation involves the insertion of tubes into the stomach or intestines for diagnostic or therapeutic purposes. This article provides an in-depth examination of GI intubation procedures, their indications, techniques, and associated clinical considerations.
Overview of Gastrointestinal Intubation
GI intubation encompasses various procedures aimed at accessing the digestive tract. These procedures are essential in managing numerous medical conditions, facilitating both diagnostic evaluations and therapeutic interventions.
Types of Gastrointestinal Intubation
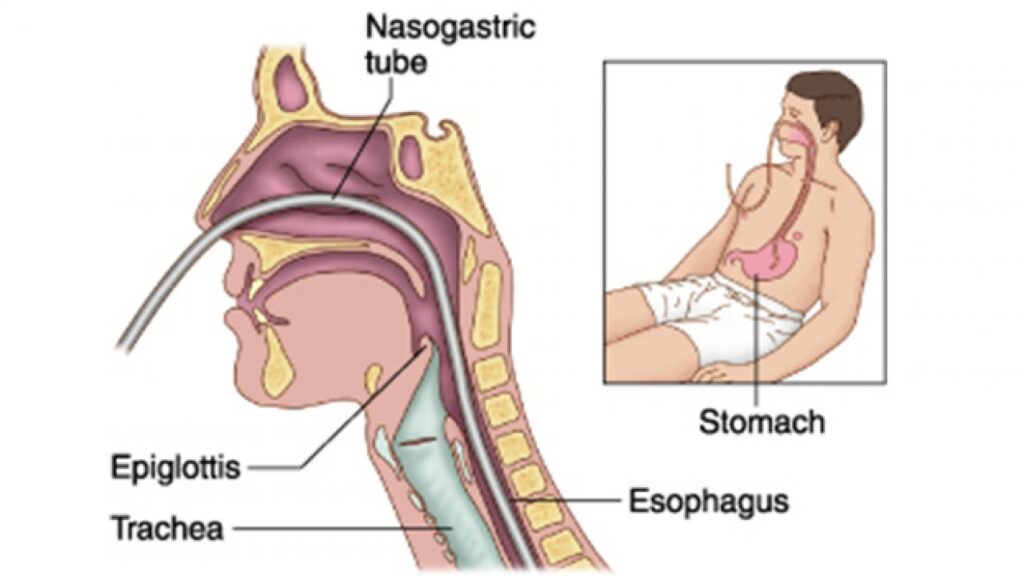
1. Nasogastric Intubation
Nasogastric (NG) intubation involves inserting a tube through the nasal passage into the stomach. This technique is commonly employed for gastric decompression, administration of medications, and enteral feeding. It is particularly useful in patients with bowel obstruction or impaired swallowing mechanisms.
2. Nasoenteric Intubation
Nasoenteric intubation extends the tube beyond the stomach into the small intestine. This approach is beneficial for patients requiring post-pyloric feeding, especially when gastric feeding is contraindicated.
Indications for Gastrointestinal Intubation
GI intubation serves multiple clinical purposes, including:
- Decompression: Relieving pressure in cases of gastric atony, ileus, or bowel obstruction.
- Nutritional Support: Providing enteral nutrition to patients unable to consume food orally.
- Medication Administration: Delivering drugs directly into the GI tract, especially in patients with swallowing difficulties.
- Diagnostic Procedures: Sampling gastric contents for analysis or administering contrast media for imaging studies.
Contraindications and Precautions
While GI intubation is generally safe, certain conditions may contraindicate its use:
- Anatomical Obstructions: Such as nasopharyngeal or esophageal blockages.
- Severe Facial Trauma: Which may complicate nasal insertion routes.
- Coagulation Disorders: Increasing the risk of bleeding during tube placement.
Careful patient assessment is crucial to mitigate potential risks.
Procedure Techniques
The technique for GI intubation varies based on the type and purpose of the procedure:
- Nasogastric Intubation: Involves measuring the appropriate tube length, lubricating the tube, and gently advancing it through the nasal passage into the stomach. Confirmation of placement is achieved through aspiration of gastric contents or radiographic imaging.
- Nasoenteric Intubation: Requires advancing the tube beyond the stomach into the small intestine, often under fluoroscopic guidance to ensure accurate placement.
Potential Complications
Although generally safe, GI intubation may be associated with complications such as:
- Misplacement: Accidental insertion into the respiratory tract, necessitating immediate correction.
- Mucosal Injury: Trauma to the nasal or esophageal lining during insertion.
- Infection: Risk of sinusitis or aspiration pneumonia if aseptic techniques are not followed.
Adherence to proper procedural protocols is essential to minimize these risks.
Gastrointestinal tract intubation is a pivotal procedure in modern medicine, facilitating a range of diagnostic and therapeutic interventions. Understanding the indications, techniques, and potential complications associated with GI intubation ensures optimal patient outcomes and enhances the efficacy of medical treatments.