Intra-abdominal Peptostreptococcus abscess is a severe infection caused by anaerobic bacteria, primarily Peptostreptococcus species. These infections often develop secondary to intra-abdominal conditions such as perforated appendicitis, diverticulitis, or post-surgical complications. Due to the anaerobic nature of Peptostreptococcus, these abscesses require prompt medical intervention, including imaging, drainage, and targeted antibiotic therapy.
Causes and Pathophysiology
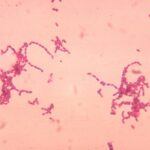
Peptostreptococcus species are gram-positive anaerobic cocci that reside in the normal human flora, particularly in the gastrointestinal tract. When the integrity of the mucosal barrier is compromised, these bacteria can translocate into sterile peritoneal or retroperitoneal spaces, leading to abscess formation.
Risk Factors
- Perforated appendicitis or diverticulitis
- Gastrointestinal surgery complications
- Trauma or penetrating abdominal injuries
- Immunosuppressive conditions (e.g., diabetes, cancer, HIV/AIDS)
- Bowel ischemia or infarction
Clinical Presentation
The symptoms of intra-abdominal Peptostreptococcus abscess depend on the location and severity of the infection. Common manifestations include:
- Persistent abdominal pain and tenderness
- Fever and chills
- Nausea and vomiting
- Localized or diffuse peritonitis
- Leukocytosis with left shift (elevated white blood cell count)
- Anorexia and weight loss in chronic cases
Diagnosis
Accurate diagnosis is crucial for effective management. The following diagnostic modalities are commonly used:
1. Laboratory Tests
- Complete blood count (CBC) with differential
- Blood cultures for aerobic and anaerobic organisms
- C-reactive protein (CRP) and procalcitonin levels
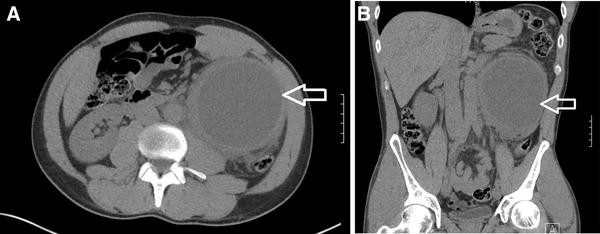
2. Imaging Studies
- Ultrasound (USG): Initial modality for detecting fluid collections.
- Computed Tomography (CT) Scan: Gold standard for identifying abscess location, size, and surrounding structures.
- Magnetic Resonance Imaging (MRI): Useful for complex cases, especially in retroperitoneal abscesses.
3. Microbiological Analysis
- Aspiration and Culture: Direct sampling of the abscess fluid for anaerobic culture and antimicrobial susceptibility testing.
- Gram Stain and PCR: Helps in identifying mixed polymicrobial infections.
Treatment Approach
Management of intra-abdominal Peptostreptococcus abscess involves a combination of surgical and pharmacological interventions.
1. Abscess Drainage
- Percutaneous Drainage (PCD): Image-guided needle aspiration for small-to-moderate abscesses.
- Surgical Drainage: Laparotomy or laparoscopy for large or multiloculated abscesses.
2. Antibiotic Therapy
Empirical broad-spectrum antibiotics should cover anaerobic and facultative organisms. Once culture results are available, targeted therapy can be initiated.
- Empirical Therapy:
- Piperacillin-Tazobactam or Meropenem
- Metronidazole in combination with a third-generation cephalosporin (Ceftriaxone)
- Definitive Therapy: Based on susceptibility testing, options include Clindamycin or Ampicillin-Sulbactam.
- Duration: Typically 4-6 weeks, depending on response and resolution of symptoms.
3. Supportive Care
- Intravenous fluids to maintain hemodynamic stability
- Nutritional support in severe or prolonged cases
- Pain management with non-opioid analgesics
Complications
If left untreated, intra-abdominal abscesses can lead to severe complications:
- Peritonitis and septic shock
- Fistula formation (e.g., enterocutaneous fistula)
- Multi-organ dysfunction syndrome (MODS)
- Recurrence or chronic infection
Prevention and Prognosis
Preventive Measures
- Prompt surgical intervention for intra-abdominal pathology
- Early initiation of antibiotics in high-risk patients
- Strict aseptic technique during abdominal surgeries
- Close postoperative monitoring for signs of infection
Prognosis
With timely diagnosis and appropriate management, the prognosis is generally favorable. However, delayed treatment or underlying comorbidities can increase mortality risk.
Intra-abdominal Peptostreptococcus abscess is a serious condition that requires early recognition and comprehensive treatment. A combination of imaging, microbiological analysis, abscess drainage, and targeted antibiotics ensures optimal patient outcomes.