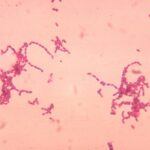
Intra-abdominal Klebsiella abscess is a serious bacterial infection caused by Klebsiella pneumoniae, a gram-negative pathogen. It typically develops due to perforated organs, post-surgical infections, or bloodstream dissemination. Prompt diagnosis and aggressive treatment are necessary to prevent complications like sepsis and multi-organ failure.
Causes and Risk Factors
- Biliary tract infections: Cholecystitis and cholangitis can lead to bacterial spread.
- Gastrointestinal perforations: Conditions like diverticulitis and peptic ulcers can introduce bacteria.
- Post-surgical infections: Abdominal surgeries, particularly bowel resections, increase risk.
- Diabetes mellitus: High glucose levels promote bacterial growth and impair immune response.
- Immunosuppression: Cancer treatment, organ transplantation, and chronic diseases lower immunity.
- Foreign body presence: Indwelling catheters and surgical mesh provide bacterial adhesion sites.
Symptoms
- Persistent fever and chills
- Severe abdominal pain and tenderness
- Nausea and vomiting
- Distended abdomen with guarding
- Signs of sepsis (hypotension, tachycardia)
- Altered mental status in severe cases
Diagnosis
Laboratory Tests
- Complete blood count (CBC): Elevated white blood cell count (leukocytosis)
- Blood cultures: Identifies bacteremia and determines antimicrobial susceptibility
- C-reactive protein (CRP) & Procalcitonin: Inflammatory markers indicating infection severity
Imaging Techniques
- Ultrasound: Initial screening tool for localized abscesses
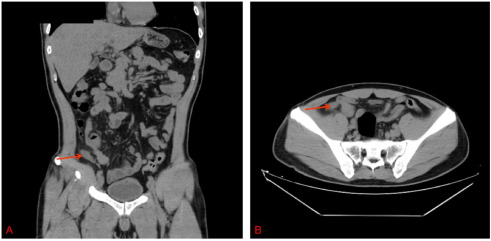
- Computed Tomography (CT) Scan: Gold standard for detecting abscesses, showing fluid collections with rim enhancement
- Magnetic Resonance Imaging (MRI): Useful for soft-tissue differentiation in complex cases
Treatment Strategies
Empirical Antibiotic Therapy
Broad-spectrum intravenous antibiotics covering gram-negative and anaerobic organisms are essential:
- First-line options: Carbapenems (meropenem, imipenem), third-generation cephalosporins (ceftriaxone), or piperacillin-tazobactam
- Combination therapy: Metronidazole for anaerobic coverage
- Resistant cases: Polymyxins or tigecycline for carbapenem-resistant Klebsiella pneumoniae
Abscess Drainage
- Percutaneous Drainage (PCD): Minimally invasive, guided by ultrasound or CT
- Surgical Drainage: Required for large, multiloculated, or inaccessible abscesses
- Laparoscopic Drainage: A less invasive surgical option in select cases
Supportive Care
- Intravenous fluid resuscitation
- Nutritional support with enteral or parenteral feeding
- Management of underlying conditions (e.g., glycemic control in diabetes)
Complications
- Sepsis and Septic Shock: Systemic inflammatory response leading to organ dysfunction
- Peritonitis: Spread of infection causing diffuse abdominal inflammation
- Multiorgan Failure: Liver, kidney, and respiratory dysfunction in severe cases
- Fistula Formation: Abnormal connections between organs due to persistent infection
Prognosis and Recovery
Early intervention improves outcomes, with mortality rates ranging from 10-30% depending on severity and comorbidities. Patients typically require prolonged antibiotic therapy (4-6 weeks), followed by close monitoring for recurrence.
Prevention
- Infection Control Measures: Strict aseptic techniques in hospital settings
- Proper Management of Chronic Conditions: Blood sugar control in diabetics, immunosuppression monitoring
- Early Treatment of Gastrointestinal Disorders: Prompt intervention for diverticulitis, ulcers, and gallbladder infections
Intra-abdominal Klebsiella abscess is a severe condition requiring timely diagnosis and aggressive management. Advanced imaging, targeted antibiotic therapy, and appropriate surgical intervention significantly improve patient outcomes. Preventative measures and early intervention play a crucial role in reducing morbidity and mortality associated with this life-threatening infection.