Intra-abdominal Clostridium abscess is a severe infection characterized by localized pus accumulation in the abdominal cavity caused by Clostridium bacteria, particularly Clostridium perfringens. These abscesses can lead to serious complications if not diagnosed and treated promptly. This article explores the etiology, clinical manifestations, diagnostic techniques, and treatment options for intra-abdominal Clostridium abscesses.
Causes and Risk Factors
Clostridium species are anaerobic, spore-forming bacteria commonly found in soil, feces, and the human gastrointestinal tract. Intra-abdominal infections occur when these bacteria invade sterile peritoneal spaces due to:
- Perforation of abdominal organs (e.g., perforated appendix, diverticulitis, gastric ulcers)
- Post-surgical infections following abdominal surgeries
- Trauma-induced intestinal rupture
- Complications of intra-abdominal malignancies
- Gastrointestinal ischemia or necrosis
Risk Factors
- Diabetes mellitus (impaired immune response)
- Immunosuppression (chemotherapy, HIV, steroids)
- Prolonged antibiotic use (disrupts gut flora balance)
- Chronic liver disease (reduced immune clearance)
Symptoms of Intra-Abdominal Clostridium Abscess
Patients with intra-abdominal Clostridium abscess may present with:
- Severe abdominal pain, particularly in the affected quadrant
- High fever and chills
- Nausea and vomiting
- Abdominal distension and tenderness
- Reduced bowel movements or ileus
- Signs of sepsis (hypotension, tachycardia)
Diagnosis
Accurate diagnosis involves a combination of clinical evaluation, imaging techniques, and laboratory tests:
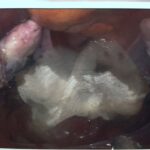
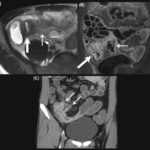
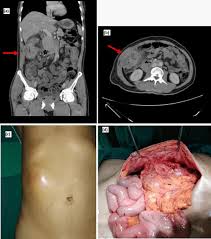
1. Imaging Studies
- CT Scan with Contrast: The gold standard for identifying abscess location and size.
- Ultrasound: Used for guided drainage procedures.
- MRI: Occasionally used for deeper abscess visualization.
2. Laboratory Tests
- Complete Blood Count (CBC): Elevated white blood cells (leukocytosis)
- Blood Cultures: To detect bacteremia
- C-reactive Protein (CRP) & Procalcitonin: Indicators of systemic inflammation
3. Microbiological Analysis
- Gram Stain & Culture: Identifies Clostridium perfringens or other Clostridium species
- Polymerase Chain Reaction (PCR): Confirms bacterial DNA presence
Treatment Approaches
Management of intra-abdominal Clostridium abscess requires a multi-faceted approach:
1. Antibiotic Therapy
Empirical broad-spectrum antibiotics covering anaerobes and facultative bacteria are initiated until culture results guide targeted therapy:
- First-line Therapy: Piperacillin-tazobactam or a combination of metronidazole with ceftriaxone
- Alternatives: Carbapenems (meropenem), clindamycin for penicillin-allergic patients
- Duration: 4–6 weeks, adjusted based on clinical response
2. Percutaneous or Surgical Drainage
- Percutaneous Drainage: CT- or ultrasound-guided catheter insertion
- Surgical Drainage: Laparotomy or laparoscopy for complex, multiloculated abscesses
3. Supportive Care
- Fluid resuscitation to maintain hemodynamic stability
- Pain management with opioids or NSAIDs
- Nutritional support via enteral or parenteral feeding if needed
Prognosis and Complications
Early detection and treatment significantly improve outcomes. However, untreated or inadequately managed infections can lead to:
- Peritonitis
- Sepsis and multi-organ failure
- Fistula formation
- Recurrence of abscess
Prevention Strategies
- Strict aseptic techniques during surgeries
- Prompt treatment of gastrointestinal infections and perforations
- Prophylactic antibiotics before abdominal surgeries
- Optimized management of chronic illnesses
Intra-abdominal Clostridium abscess is a potentially life-threatening condition requiring timely intervention. A comprehensive approach, including early diagnosis through imaging and microbiological studies, targeted antibiotic therapy, and appropriate drainage procedures, is essential for successful management. Preventive measures, including infection control and prompt surgical intervention, can reduce the incidence and severity of these abscesses.