Insulinoma is a rare, usually benign tumor of the pancreas that causes excessive insulin production, leading to recurrent episodes of hypoglycemia (low blood sugar). As a neuroendocrine tumor, insulinoma arises from the insulin-producing beta cells in the pancreas. While most insulinomas are small and non-cancerous, their ability to cause severe hypoglycemia makes early diagnosis and treatment crucial.
Understanding Insulinoma
What Is an Insulinoma?
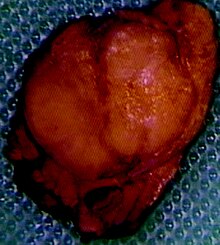
An insulinoma is a functional neuroendocrine tumor of the pancreas that secretes excessive insulin, disrupting normal glucose regulation. In most cases, insulinomas are small (less than 2 cm in diameter) and solitary. Around 90% are benign, but malignant cases, though rare, can metastasize to the liver or lymph nodes.
The Role of Insulin in the Body
Insulin is a hormone produced by the beta cells of the pancreas. It helps regulate blood glucose levels by facilitating the uptake of glucose into cells. In a healthy individual, insulin secretion is tightly controlled. However, an insulinoma produces insulin autonomously, leading to dangerously low blood sugar levels.
Causes and Risk Factors
Causes of Insulinoma
The exact cause of insulinoma remains unclear, but it is associated with genetic and endocrine disorders. Some cases occur sporadically, while others may be linked to multiple endocrine neoplasia type 1 (MEN1), a hereditary condition that increases the risk of pancreatic tumors.
Risk Factors
- Genetic predisposition: Family history of MEN1
- Gender: More common in women
- Age: Typically diagnosed in adults between 40 and 60 years
- Underlying endocrine disorders: Association with neuroendocrine tumors
Symptoms of Insulinoma
The symptoms of insulinoma result from recurrent hypoglycemia, which affects brain function and overall metabolism. These symptoms can be divided into neurogenic (autonomic) and neuroglycopenic (cerebral) manifestations.
Neurogenic Symptoms (Autonomic Dysfunction)
- Sweating
- Tremors
- Palpitations
- Anxiety
- Hunger
Neuroglycopenic Symptoms (Cognitive Impairment)
- Confusion
- Blurred vision
- Weakness
- Dizziness
- Seizures
- Loss of consciousness
The hallmark of insulinoma is the Whipple’s triad, which includes:
- Symptoms of hypoglycemia
- Blood glucose level <50 mg/dL
- Symptom relief after glucose administration
Diagnosis of Insulinoma
Clinical Assessment
A detailed patient history and physical examination focus on identifying recurrent hypoglycemia and its triggers.
Laboratory Tests
- Fasting Blood Glucose Test: Evaluates hypoglycemia after prolonged fasting
- Insulin and C-Peptide Levels: Differentiates insulinoma from exogenous insulin use
- Proinsulin Measurement: Elevated in insulinomas
Imaging Studies
- CT Scan or MRI: Detects pancreatic tumors
- Endoscopic Ultrasound (EUS): Provides high-resolution imaging of small insulinomas
- Selective Arterial Calcium Stimulation Test: Confirms excessive insulin secretion
Differential Diagnosis
Insulinoma must be distinguished from other causes of hypoglycemia, such as:
- Reactive hypoglycemia (postprandial hypoglycemia)
- Exogenous insulin administration
- Adrenal insufficiency
- Insulin-like growth factor (IGF)-secreting tumors
Treatment of Insulinoma
Surgical Treatment
Surgical removal is the definitive treatment for insulinoma, with a high success rate. The approach depends on tumor size and location:
- Enucleation: Used for small, well-defined tumors
- Partial Pancreatectomy: Required for multiple or deeply embedded tumors
Medical Management
For inoperable or recurrent cases, medical therapy is necessary:
- Diazoxide: Reduces insulin secretion
- Somatostatin Analogues (Octreotide): Inhibits insulin release
- Everolimus: Used in malignant cases
Dietary and Supportive Care
- Frequent small meals to maintain glucose levels
- Avoidance of simple sugars that trigger rapid insulin spikes
- Continuous glucose monitoring for high-risk patients
Prognosis and Long-Term Outlook
- Benign insulinomas have an excellent prognosis after surgical removal, with low recurrence rates.
- Malignant insulinomas, though rare, require ongoing monitoring and targeted therapies.
- Early diagnosis and treatment significantly improve quality of life and prevent life-threatening hypoglycemia.
Insulinoma is a rare but potentially life-threatening condition that requires prompt diagnosis and management. With advances in diagnostic imaging and surgical techniques, most patients achieve a full recovery. Awareness of symptoms, early testing, and specialized care are crucial for optimal outcomes.

