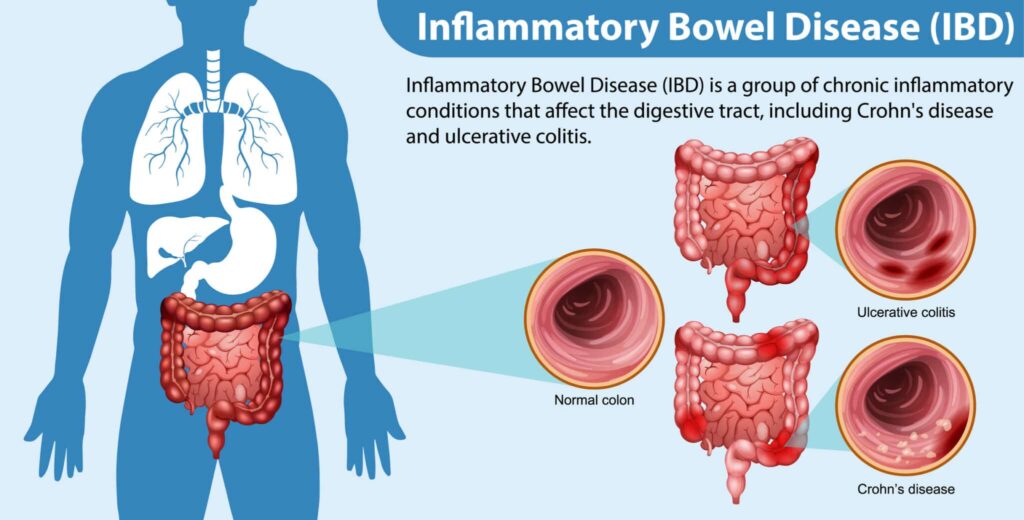
Inflammatory Bowel Disease (IBD) is a chronic condition that causes inflammation in the digestive tract. It primarily includes two disorders: Crohn’s disease and ulcerative colitis. These conditions result in abdominal pain, diarrhea, weight loss, and fatigue, significantly affecting a person’s quality of life.
Types of Inflammatory Bowel Disease
Crohn’s Disease
- Affects any part of the gastrointestinal (GI) tract from the mouth to the anus.
- Causes inflammation through multiple layers of the bowel wall.
- Symptoms include abdominal cramps, persistent diarrhea, and weight loss.
Ulcerative Colitis
- Affects only the colon and rectum.
- Inflammation occurs in the innermost lining of the colon.
- Symptoms include bloody diarrhea, urgency, and abdominal discomfort.
Causes of Inflammatory Bowel Disease
Genetic Factors
- Family history increases susceptibility to IBD.
- Certain genetic mutations are linked to the disease’s development.
Immune System Dysfunction
- An abnormal immune response mistakenly attacks healthy cells in the GI tract.
Environmental Triggers
- Smoking, diet, and stress may exacerbate symptoms.
- Industrialized regions show higher prevalence rates, suggesting environmental factors.
Symptoms of Inflammatory Bowel Disease
- Abdominal pain and cramping
- Chronic diarrhea
- Blood in stool
- Unintended weight loss
- Fatigue and weakness
- Fever in severe cases
Diagnosis of Inflammatory Bowel Disease
Blood Tests
- Detect anemia or signs of infection.
Stool Tests
- Identify inflammation markers and rule out infections.
Endoscopic Procedures
- Colonoscopy: Visualizes the entire colon.
- Sigmoidoscopy: Focuses on the rectum and lower colon.
Imaging Studies
- CT Scan and MRI: Help detect inflammation, fistulas, or abscesses.
Treatment Options for Inflammatory Bowel Disease
Medications
- Anti-inflammatory drugs: 5-aminosalicylates and corticosteroids.
- Immune system suppressors: Azathioprine, methotrexate, and biologics.
- Antibiotics: Treat bacterial infections and abscesses.
Lifestyle Modifications
- Diet adjustments with low-residue and anti-inflammatory foods.
- Stress management techniques like yoga and meditation.
Surgery
- In severe cases, surgery may involve bowel resection or colectomy.
Complications of Inflammatory Bowel Disease
- Bowel obstruction
- Malnutrition
- Colon cancer
- Abscesses and fistulas
Preventive Measures
- Maintain a balanced diet rich in fiber, fruits, and vegetables.
- Avoid smoking and excessive alcohol consumption.
- Regular check-ups for early detection and better management.
Living with Inflammatory Bowel Disease
Managing IBD requires consistent medical care, lifestyle adjustments, and mental well-being practices. Support groups and professional counseling can greatly improve a patient’s quality of life.
FAQs
What is the difference between Crohn’s disease and ulcerative colitis?
Crohn’s disease can affect any part of the GI tract, while ulcerative colitis is confined to the colon and rectum.
Can IBD be cured?
There is no known cure for IBD, but symptoms can be managed effectively with proper treatment.
Is IBD the same as IBS?
No, IBD involves inflammation and potential intestinal damage, while IBS is a functional disorder without inflammation.
Are there dietary recommendations for IBD patients?
Yes, a low-fiber diet during flare-ups and an anti-inflammatory diet during remission can help manage symptoms.
What triggers IBD flare-ups?
Stress, certain medications, infections, and dietary choices may trigger flare-ups.

