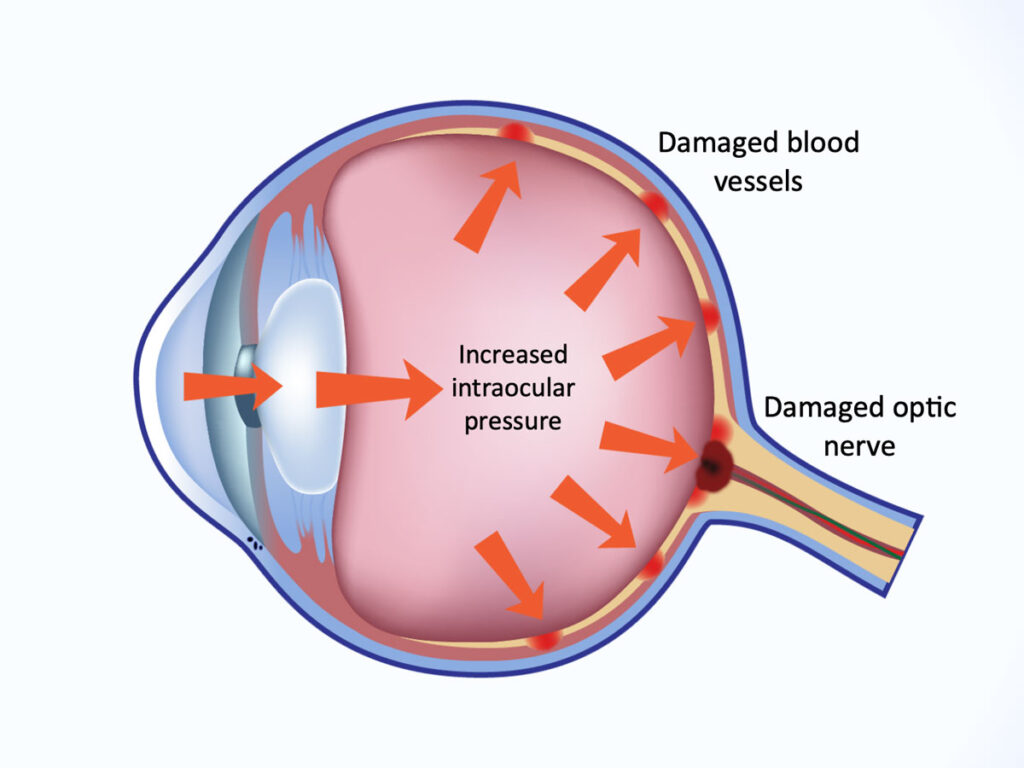
Increased intraocular pressure (IOP) following an ocular procedure is a common yet significant concern in ophthalmology. Elevated IOP can pose risks to ocular health, potentially leading to optic nerve damage and vision loss. Understanding the underlying causes, risk factors, and management strategies is crucial for ensuring patient safety and successful post-operative outcomes.
What is Intraocular Pressure (IOP)?
Intraocular pressure refers to the fluid pressure within the eye. Normal IOP typically ranges between 10-21 mmHg. Pressure levels exceeding this range may cause complications, particularly following ocular surgery or procedures.
Causes of Increased IOP After Ocular Procedures
Several factors may contribute to increased IOP after ocular interventions:
1. Steroid Response
- Post-operative corticosteroids used to manage inflammation may induce a steroid response, leading to increased aqueous humor production or reduced outflow.
2. Retained Viscoelastic Agents
- During cataract or glaucoma surgery, residual viscoelastic material can obstruct the trabecular meshwork, impeding aqueous outflow and raising IOP.
3. Intraocular Gas Bubbles
- In vitrectomy procedures, intraocular gas bubbles may expand, particularly with altitude changes, increasing pressure within the eye.
4. Hyphema Formation
- Blood accumulation in the anterior chamber can elevate IOP by obstructing the trabecular meshwork.
5. Pupillary Block
- In certain procedures such as lens implantation, misalignment may block aqueous humor flow through the pupil, resulting in pressure buildup.
6. Inflammatory Response
- Post-surgical inflammation can cause trabecular meshwork dysfunction, reducing aqueous humor outflow.
Risk Factors for Elevated IOP Post-Procedure
Patients with the following conditions are at higher risk of developing increased IOP:
- Pre-existing glaucoma
- High myopia
- History of ocular hypertension
- Dense cataracts requiring prolonged surgery
- Complicated surgical procedures
Symptoms of Elevated IOP
Patients experiencing post-operative IOP spikes may report:
- Eye pain or discomfort
- Blurred vision
- Headache or brow ache
- Halos around lights
- Nausea and vomiting (in severe cases)
Diagnostic Procedures
Accurate diagnosis of increased IOP involves:
- Tonometry: Measures IOP levels.
- Gonioscopy: Evaluates the drainage angle.
- Ophthalmoscopy: Assesses optic nerve damage.
- Anterior Segment Optical Coherence Tomography (OCT): Provides detailed imaging of anterior eye structures.
Management and Treatment Options
Effective management strategies for elevated IOP include:
1. Medications
- Beta-Blockers: Reduce aqueous humor production.
- Alpha Agonists: Decrease aqueous humor formation and enhance outflow.
- Prostaglandin Analogs: Improve uveoscleral outflow.
- Carbonic Anhydrase Inhibitors: Lower fluid production.
- Osmotic Agents: Emergency treatment to rapidly reduce IOP.
2. Surgical Interventions
- Anterior Chamber Paracentesis: Immediate relief by aspirating aqueous humor.
- Laser Procedures: Such as YAG laser iridotomy for pupillary block.
- Trabeculectomy: Enhances aqueous outflow for persistent pressure issues.
3. Lifestyle and Recovery Measures
- Elevating the head during sleep to facilitate fluid drainage.
- Avoiding strenuous activities that may increase pressure.
- Close monitoring for several weeks following surgery.
Preventive Measures
- Careful removal of viscoelastic agents during surgery.
- Judicious use of post-operative steroids with regular IOP monitoring.
- Proper patient education on symptoms and follow-up care.
Complications of Untreated Elevated IOP
Failure to manage increased IOP can lead to:
- Optic nerve damage
- Progressive visual field loss
- Development or worsening of glaucoma
- Permanent vision impairment
Managing increased intraocular pressure after ocular procedures is essential for preserving vision and preventing complications. Early diagnosis, proactive treatment, and preventive strategies are key to ensuring optimal outcomes. Ophthalmologists must tailor treatment approaches to each patient’s needs, considering their medical history and surgical factors.