Inclusion body myositis (IBM) is a rare, progressive muscle disorder characterized by inflammation, muscle weakness, and degeneration. IBM primarily affects older adults, typically over the age of 50, and is more common in men than women. The condition is classified as an idiopathic inflammatory myopathy (IIM) and is distinct due to its slow progression and resistance to conventional treatments.
Causes of Inclusion Body Myositis
The exact cause of IBM remains unknown; however, it is believed to result from a combination of autoimmune and degenerative processes. Key contributing factors may include:
- Autoimmune response: The immune system mistakenly attacks muscle tissues, causing chronic inflammation.
- Protein abnormalities: Abnormal protein accumulation, such as beta-amyloid and TDP-43, is often seen in affected muscle fibers.
- Genetic predisposition: While IBM is generally not hereditary, certain genetic factors may increase susceptibility.
Symptoms of Inclusion Body Myositis
IBM develops gradually and symptoms may vary. Common signs include:
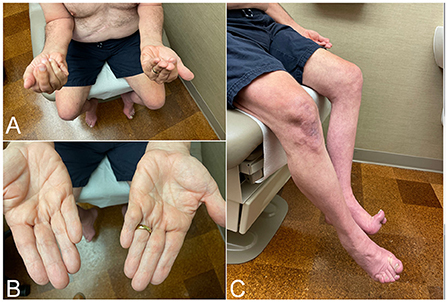
- Progressive muscle weakness, particularly in the quadriceps and forearm muscles
- Difficulty gripping objects or performing fine motor tasks
- Muscle atrophy and reduced hand function
- Trouble swallowing (dysphagia)
- Impaired mobility and increased risk of falls
Diagnosis of Inclusion Body Myositis
Diagnosing IBM can be challenging due to its slow progression and symptom overlap with other muscle disorders. The following diagnostic methods are employed:
1. Physical Examination
Neurologists assess muscle strength, coordination, and reflexes to identify characteristic weaknesses.
2. Blood Tests
- Elevated creatine kinase (CK) levels indicate muscle damage.
- Presence of specific autoantibodies like anti-cN1A is common in IBM cases.
3. Electromyography (EMG)
EMG studies detect abnormal electrical activity in muscles, confirming dysfunction.
4. Muscle Biopsy
A muscle biopsy is the most definitive diagnostic method for IBM. Key indicators include:
- Inflammatory cell infiltration
- Vacuoles containing protein deposits
- Rimmed vacuoles with abnormal protein accumulation
5. Magnetic Resonance Imaging (MRI)
MRI scans help visualize muscle inflammation and atrophy patterns distinctive to IBM.
Treatment for Inclusion Body Myositis
While there is no known cure for IBM, management strategies focus on symptom control and improving quality of life. Common treatment options include:
1. Physical Therapy
Customized exercise programs enhance mobility, balance, and muscle strength. Stretching routines are essential to reduce stiffness and improve flexibility.
2. Occupational Therapy
Assistive devices, such as braces or grab bars, aid in performing daily activities.
3. Speech Therapy
For patients with dysphagia, speech therapists provide exercises to improve swallowing.
4. Medications
- Immunosuppressants: While generally less effective in IBM, medications such as corticosteroids may temporarily reduce inflammation.
- Intravenous Immunoglobulin (IVIG): Used in select cases to improve muscle strength and reduce inflammation.
5. Lifestyle Modifications
Balanced nutrition, weight management, and muscle-strengthening exercises play vital roles in managing IBM symptoms.
Prognosis of Inclusion Body Myositis
IBM is a chronic condition with a slow progression. While it rarely shortens life expectancy, it can significantly affect mobility and independence. Early intervention through physical therapy and lifestyle adaptations can greatly improve quality of life.
Prevention of Inclusion Body Myositis
As the exact cause remains unclear, there are no definitive preventive measures. However, maintaining an active lifestyle, avoiding excessive stress on muscles, and seeking early medical evaluation for persistent weakness may reduce the risk of severe complications.
FAQs:
1. Is inclusion body myositis fatal?
IBM itself is not typically fatal but can severely impact quality of life and mobility.
2. Can inclusion body myositis be cured?
Currently, there is no cure for IBM. Treatment focuses on symptom management and improved mobility.
3. What is the life expectancy with IBM?
Life expectancy is generally normal; however, disability levels can progress over time.
4. How is inclusion body myositis different from other myopathies?
IBM progresses slowly, affects older adults, and shows characteristic muscle degeneration with protein deposits.
5. Are there clinical trials for IBM treatments?
Yes, ongoing research explores new therapies such as anti-inflammatory drugs, gene therapies, and regenerative medicine.
Inclusion body myositis is a complex condition requiring multidisciplinary management. Early diagnosis and comprehensive care strategies are key to improving outcomes for individuals affected by this disorder.