Impetigo is a common and highly contagious bacterial skin infection that predominantly affects infants and young children. It manifests as red sores that rupture, ooze fluid, and eventually develop a yellow-brown crust. Although impetigo is not typically serious, it can be uncomfortable and requires appropriate treatment to prevent complications and spreading.

Causes of Impetigo
Impetigo is caused by two primary bacterial strains:
- Staphylococcus aureus
- Streptococcus pyogenes (Group A Streptococcus)
These bacteria often enter the skin through:
- Cuts, insect bites, or scratches
- Skin conditions like eczema or dermatitis
- Contact with contaminated items such as towels, clothing, or toys
Types of Impetigo
There are three primary types of impetigo:
1. Non-Bullous Impetigo
- Most common type
- Presents as red sores that rupture quickly, leaving honey-colored crusts
- Often seen around the nose and mouth
2. Bullous Impetigo
- Characterized by larger fluid-filled blisters
- Common in young children and infants
- Often appears on the torso, arms, or legs
3. Ecthyma
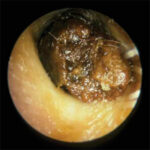
- Severe form of impetigo that penetrates deeper into the skin
- Causes painful ulcers covered with a hard, thick crust
Symptoms of Impetigo
The symptoms vary depending on the type but commonly include:
- Red sores or blisters that burst and develop crusts
- Itching and irritation
- Swollen lymph nodes near the infection site
- Mild fever in some cases
How is Impetigo Diagnosed?
Healthcare providers can typically diagnose impetigo through visual examination. In cases of severe or recurrent infections, a sample may be taken from the sores to identify the responsible bacteria and determine the most effective antibiotic treatment.
Treatment Options for Impetigo
Treatment for impetigo aims to eliminate the infection, reduce symptoms, and prevent its spread.
1. Topical Antibiotics
- Mupirocin (Bactroban) and Retapamulin (Altabax) are commonly prescribed.
- Applied directly to the affected area 2-3 times daily for up to 10 days.
2. Oral Antibiotics
- Recommended for severe or widespread impetigo cases.
- Common options include cephalexin, dicloxacillin, or clindamycin.
3. Home Remedies
While medical treatment is crucial, home remedies can support healing:
- Warm compresses to soften crusts
- Antiseptic washes to cleanse infected areas
- Avoiding scratching to prevent spreading
Prevention Strategies for Impetigo
To reduce the risk of impetigo, consider the following preventive measures:
- Frequent handwashing with soap and water
- Keeping cuts and wounds clean with antiseptics
- Avoiding close contact with infected individuals
- Disinfecting personal items like towels, bedding, and clothing
- Encouraging children to avoid scratching scabs or blisters
When to See a Doctor
Seek medical advice if you notice:
- Persistent or worsening sores
- Signs of spreading infection, such as swollen lymph nodes
- Fever or fatigue associated with skin sores
Prompt treatment can prevent complications like cellulitis, kidney inflammation, or scarring.
FAQs
1. Is impetigo contagious?
Yes, impetigo is highly contagious and can spread through skin contact or contaminated objects.
2. Can adults get impetigo?
Although impetigo is more common in children, adults can contract it, especially in crowded environments or if they have compromised skin barriers.
3. How long does impetigo last?
With treatment, impetigo typically improves within 7-10 days. Untreated cases may persist longer.
4. Can impetigo heal without antibiotics?
Mild cases may resolve without antibiotics, but treatment is recommended to reduce discomfort, prevent spreading, and speed up recovery.
5. Can impetigo cause scars?
Non-bullous impetigo rarely causes scarring, but ecthyma can leave marks due to deeper skin damage.
Impetigo is a common yet manageable bacterial infection. Early diagnosis, effective treatment, and diligent preventive measures are crucial for controlling its spread. If you suspect impetigo, consult a healthcare professional for appropriate care and guidance.