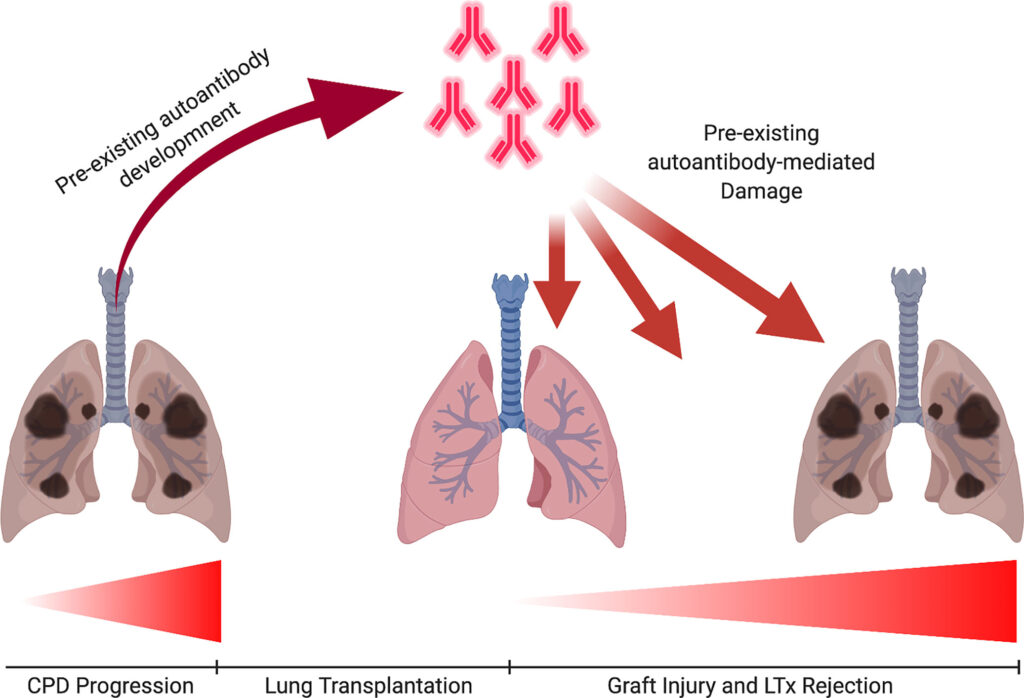
Lung transplantation is a critical intervention for patients with end-stage respiratory diseases. However, the success of such procedures heavily relies on effective immunosuppression therapy to prevent organ rejection. Immunosuppressive regimens are designed to balance rejection prevention with minimizing adverse effects like infection and malignancy.
Goals of Immunosuppression Therapy
- Prevent Acute and Chronic Rejection: Ensuring the immune system does not attack the transplanted lung.
- Reduce Infection Risk: By carefully controlling immune suppression levels.
- Minimize Drug Toxicity: Using optimal dosing strategies.
Phases of Immunosuppression Therapy
Immunosuppression therapy generally follows three key phases:
1. Induction Therapy
Induction therapy involves intense immunosuppression administered during or immediately after surgery. This phase reduces the risk of early organ rejection.
Common Induction Agents:
- Basiliximab (IL-2 receptor antagonist)
- Anti-thymocyte Globulin (ATG)
- Alemtuzumab (monoclonal antibody)
2. Maintenance Therapy
Maintenance therapy is essential for long-term rejection prevention and involves a combination of immunosuppressants.
Key Drugs for Maintenance Therapy:
- Calcineurin Inhibitors (CNIs): Tacrolimus, Cyclosporine
- Antiproliferative Agents: Mycophenolate Mofetil, Azathioprine
- Corticosteroids: Prednisone
3. Anti-rejection Therapy
In cases of acute rejection, patients may require additional treatments.
Therapeutic Agents for Rejection Management:
- High-dose Corticosteroids
- Plasmapheresis
- Intravenous Immunoglobulin (IVIG)
- Rituximab for antibody-mediated rejection
Immunosuppressive Drug Classes and Their Roles
Calcineurin Inhibitors (CNIs)
- Tacrolimus: Preferred due to superior rejection prevention rates.
- Cyclosporine: Effective but requires frequent monitoring.
Antiproliferative Agents
- Mycophenolate Mofetil (MMF): Reduces lymphocyte proliferation.
- Azathioprine: Used as an alternative to MMF.
Corticosteroids
- Essential in the early post-transplant phase for inflammation control.
mTOR Inhibitors
- Sirolimus and Everolimus: Effective in reducing chronic rejection risks but may increase the risk of delayed wound healing.
Immunosuppression Regimen Strategies
Standard Triple Therapy
- Tacrolimus + Mycophenolate Mofetil + Prednisone
- Balances efficacy with manageable side effects.
Tailored Regimens
- Adjustments based on patient-specific factors like infection risk, renal function, and comorbidities.
Potential Complications of Immunosuppression Therapy
While essential, immunosuppressive drugs carry significant risks:
- Infections: Due to weakened immune response.
- Malignancies: Higher risk of post-transplant lymphoproliferative disorder (PTLD).
- Organ Toxicity: Nephrotoxicity from CNIs, hepatotoxicity, and metabolic disturbances.
Monitoring and Follow-up
Effective monitoring helps ensure treatment success while minimizing side effects:
- Drug Levels: Frequent monitoring of tacrolimus or cyclosporine levels.
- Pulmonary Function Tests (PFTs): To detect early signs of rejection.
- Biopsy: As a gold standard for diagnosing rejection.
Immunosuppressive Therapy and Long-Term Outcomes
Long-term success hinges on balancing immunosuppression with infection control strategies. Emerging therapies, such as cell-based treatments and personalized medicine approaches, continue to improve outcomes.
Immunosuppression therapy is vital for maintaining lung transplant viability. By leveraging a carefully structured regimen, physicians can minimize rejection risks while reducing complications. Advances in immunotherapy continue to improve outcomes for lung transplant recipients.