Lung transplantation is a life-saving procedure for patients with end-stage respiratory conditions. Immunosuppression maintenance therapy is essential to prevent organ rejection and ensure long-term graft survival. This article details the strategies, drug classes, and management protocols for effective immunosuppression in lung transplant recipients.
Importance of Immunosuppression Maintenance Therapy
Due to the high immunogenicity of lung tissue and constant exposure to environmental pathogens, lung transplant recipients require stringent immunosuppression maintenance therapy. The regimen aims to:
- Prevent acute and chronic rejection
- Balance immunosuppression to minimize infection risk
- Optimize long-term organ function
Immunosuppressive Drug Classes
1. Calcineurin Inhibitors (CNIs)
- Tacrolimus: Preferred due to improved efficacy in lung transplant patients.
- Cyclosporine: An alternative for patients intolerant to tacrolimus.
2. Antiproliferative Agents
- Mycophenolate Mofetil (MMF): Widely used due to its favorable safety profile.
- Azathioprine: An alternative with comparable efficacy.
3. Corticosteroids
- Prednisone: Essential during the early post-transplant period and for managing rejection episodes.
4. mTOR Inhibitors
- Sirolimus and Everolimus: Effective in preventing chronic lung allograft dysfunction (CLAD).
5. Costimulation Blockers
- Belatacept: Used in select cases to minimize nephrotoxicity.
Standard Immunosuppression Protocols
Induction Therapy
- Administered perioperatively to prevent early rejection.
- Agents such as basiliximab or alemtuzumab are commonly used.
Maintenance Therapy Regimen
A typical maintenance protocol includes:
- Tacrolimus (trough levels: 8-12 ng/mL initially, reduced over time)
- Mycophenolate Mofetil (1-2 g/day)
- Prednisone (initially high doses, tapered gradually)
Combination Strategies
Combination therapy minimizes toxicity while enhancing efficacy. Typical regimens involve:
- CNI + Antiproliferative agent + Corticosteroid
- mTOR inhibitor added in cases of renal dysfunction or chronic rejection.
Monitoring and Dose Adjustments
Monitoring Parameters
- Drug trough levels for CNIs and mTOR inhibitors.
- Complete blood count (CBC) and liver function tests (LFTs) for antiproliferative agents.
- Renal function to prevent nephrotoxicity.
Adverse Effect Management
- Infection control: Prophylactic antibiotics and antifungal agents.
- Cancer surveillance: Due to heightened malignancy risk.
- Cardiovascular monitoring: To manage hypertension and lipid abnormalities.
Managing Complications
Acute Rejection
- Treated with high-dose corticosteroids or T-cell depleting agents such as antithymocyte globulin.
Chronic Lung Allograft Dysfunction (CLAD)
- Switching from CNIs to mTOR inhibitors may improve outcomes.
- Addition of azithromycin is common for its anti-inflammatory effects.
Opportunistic Infections
- Cytomegalovirus (CMV): Managed with valganciclovir.
- Pneumocystis jirovecii pneumonia (PJP): Prevented with trimethoprim-sulfamethoxazole.
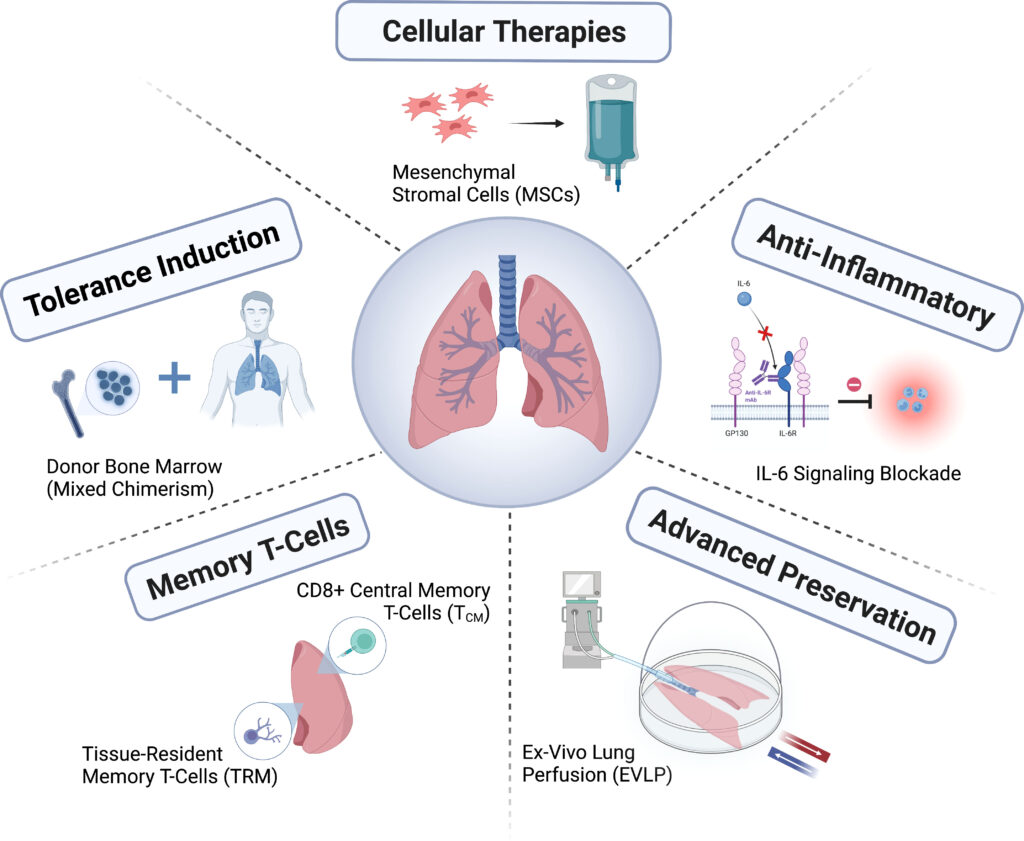
Future Directions and Emerging Therapies
- Cell-based therapies to promote tolerance.
- Biomarker-driven protocols for personalized immunosuppression management.
- Development of novel agents targeting specific immune pathways.
Immunosuppression maintenance therapy for lung transplantation requires careful balancing of efficacy and safety. By combining appropriate agents, monitoring closely, and managing complications effectively, clinicians can optimize graft survival and enhance patient outcomes.
FAQs
What is the most effective immunosuppressant for lung transplantation?
Tacrolimus combined with mycophenolate mofetil and prednisone is considered the gold standard for maintenance therapy.
How often should drug levels be monitored in lung transplant patients?
Tacrolimus levels should be monitored weekly initially, then biweekly or monthly as the patient stabilizes.
Can immunosuppression therapy be reduced over time?
Yes, immunosuppressant doses are typically tapered once the patient reaches long-term stability, with close monitoring for signs of rejection.
What is the role of mTOR inhibitors in lung transplantation?
mTOR inhibitors like sirolimus are used in cases of renal dysfunction or chronic rejection to reduce CNI-related toxicity.
How are infections managed in lung transplant recipients?
Prophylactic antibiotics, antifungal agents, and antiviral drugs are standard preventive measures, with close monitoring for opportunistic infections.