Idiopathic Intracranial Hypertension (IIH), also known as benign intracranial hypertension or pseudotumor cerebri, is a condition characterized by increased pressure inside the skull without an apparent cause. It primarily affects overweight women of childbearing age but can occur in individuals of any age or gender.
Causes of Idiopathic Intracranial Hypertension
While the exact cause of IIH remains unknown, several risk factors have been linked to the condition:
- Obesity: Individuals with a higher body mass index (BMI) are at greater risk.
- Medications: Certain drugs such as tetracyclines, vitamin A derivatives, and hormonal treatments may contribute.
- Hormonal Imbalance: Conditions like polycystic ovary syndrome (PCOS) are often associated with IIH.
- Sleep Apnea: Disrupted breathing during sleep may increase intracranial pressure.
Symptoms of Idiopathic Intracranial Hypertension
IIH symptoms can vary but often include:
- Severe Headaches: Often worse in the morning or when lying down.
- Visual Disturbances: Blurred vision, double vision, or brief visual obscurations.
- Pulsatile Tinnitus: Hearing a rhythmic, whooshing sound in the ears.
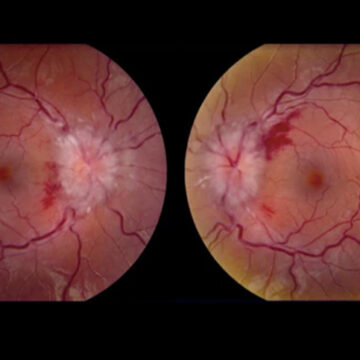
- Papilledema: Swelling of the optic nerve, which can lead to vision loss if untreated.
- Nausea and Vomiting: Resulting from increased intracranial pressure.
Diagnosing Idiopathic Intracranial Hypertension
Effective diagnosis requires a combination of clinical evaluation and diagnostic tests:
- Medical History and Physical Examination: Identifying risk factors and assessing symptoms.
- Ophthalmologic Examination: Checking for papilledema and visual disturbances.
- Lumbar Puncture (Spinal Tap): Measuring cerebrospinal fluid (CSF) pressure to confirm elevated intracranial pressure.
- Neuroimaging (MRI or CT Scan): Ruling out brain tumors or structural abnormalities.
Treatment Options for Idiopathic Intracranial Hypertension
Managing IIH involves reducing intracranial pressure and alleviating symptoms. Treatment strategies include:
Medications
- Acetazolamide: A carbonic anhydrase inhibitor that reduces CSF production.
- Topiramate: Often used to control headaches and aid in weight loss.
- Diuretics: Assist in fluid reduction to decrease pressure.
Lifestyle Modifications
- Weight Loss: Reducing body weight by 5-10% can significantly improve symptoms.
- Dietary Changes: Limiting salt intake and adopting a healthy diet.
Surgical Interventions
- Optic Nerve Sheath Fenestration (ONSF): A procedure to relieve pressure on the optic nerve.
- Shunt Surgery: Placement of a shunt to drain excess CSF.
Therapeutic Procedures
- Lumbar Punctures: Regular spinal taps may help control pressure.
- Venous Sinus Stenting: A less common but effective treatment for patients with venous sinus stenosis.
Long-Term Management and Prognosis
- Follow-Up Care: Regular eye exams and neurological evaluations are essential.
- Vision Monitoring: Prompt treatment can prevent permanent vision loss.
- Lifestyle Commitment: Sustained weight management and a healthy lifestyle are crucial for long-term symptom control.
Frequently Asked Questions:
What triggers idiopathic intracranial hypertension?
IIH is often linked to obesity, hormonal imbalances, and certain medications. Identifying and managing these factors can reduce the risk.
Can idiopathic intracranial hypertension be cured?
While IIH may not have a definitive cure, effective management through medications, lifestyle changes, and procedures can successfully control symptoms.
Is idiopathic intracranial hypertension life-threatening?
IIH is typically not life-threatening but can cause permanent vision loss if untreated.
How does weight loss impact IIH?
Weight loss is one of the most effective strategies for reducing intracranial pressure and alleviating IIH symptoms.
What is the prognosis for IIH patients?
With appropriate treatment and lifestyle adjustments, many patients experience significant improvement and long-term symptom control.
Idiopathic Intracranial Hypertension requires early diagnosis and comprehensive management to prevent complications like vision loss. By understanding its causes, symptoms, and treatment options, patients can effectively manage this condition with improved quality of life.