Bradycardia is a condition characterized by a slower-than-normal heart rate, typically defined as fewer than 60 beats per minute in adults. While a slow heart rate can be a sign of excellent physical fitness in some individuals, it may also indicate underlying health concerns requiring medical attention. This article delves into the causes, symptoms, diagnostic procedures, treatment options, and preventive strategies related to bradycardia.
What Is Bradycardia?
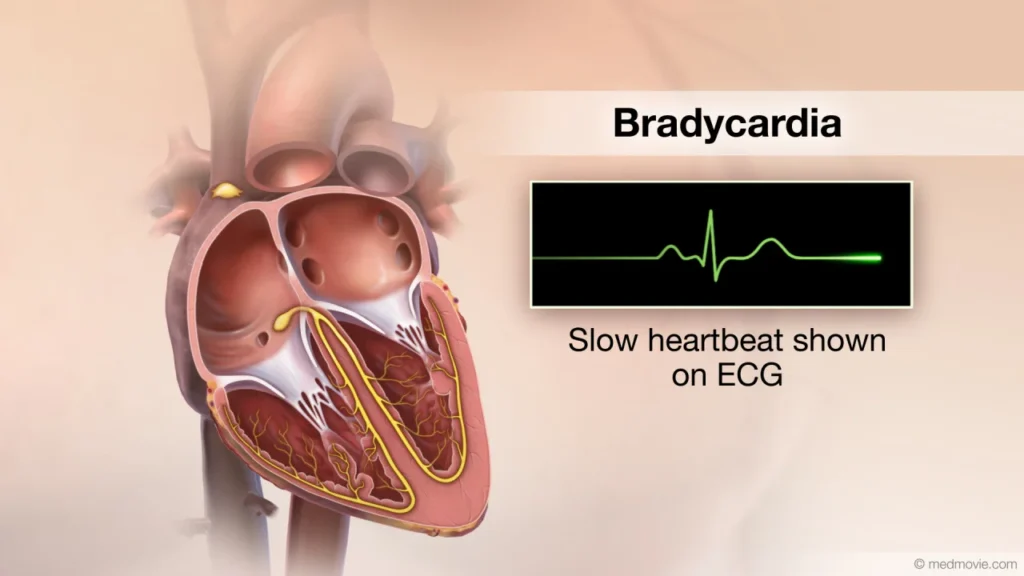
Bradycardia originates from the Greek words “bradys,” meaning slow, and “kardia,” meaning heart. The heart’s electrical system regulates its rhythm, and any disruption to this system can result in bradycardia. In severe cases, the condition can impede the heart’s ability to pump enough oxygen-rich blood to the body, leading to fatigue, dizziness, or even more serious complications.
Causes of Bradycardia
Bradycardia may arise from a variety of factors, including:
Intrinsic Causes
- Aging-Related Changes: Degeneration of the heart’s electrical pathways due to aging.
- Heart Conditions: Damage from heart disease, myocardial infarction, or cardiomyopathy.
- Congenital Heart Defects: Structural abnormalities present from birth.
- Sinus Node Dysfunction: Malfunction of the heart’s natural pacemaker.
Extrinsic Causes
- Medications: Drugs like beta-blockers, calcium channel blockers, or antiarrhythmics.
- Electrolyte Imbalances: Abnormal levels of potassium, calcium, or magnesium.
- Hypothyroidism: An underactive thyroid gland slowing metabolic processes.
- Sleep Apnea: Interrupted breathing during sleep affecting heart rhythms.
- Infections: Conditions such as Lyme disease or myocarditis.
Symptoms of Bradycardia
Symptoms can vary depending on the severity of the condition and the individual’s overall health. Common signs include:
- Fatigue and weakness
- Dizziness or lightheadedness
- Shortness of breath
- Fainting (syncope)
- Chest pain
- Confusion or memory problems
- Exercise intolerance
Diagnosing Bradycardia
Healthcare providers use a combination of patient history, physical examination, and diagnostic tests to confirm bradycardia. Key diagnostic methods include:
- Electrocardiogram (ECG): Measures the heart’s electrical activity.
- Holter Monitor: A portable device worn to track heart rhythms over 24-48 hours.
- Event Recorder: Used for monitoring sporadic symptoms.
- Echocardiogram: Visualizes heart structure and function.
- Blood Tests: Checks for electrolyte imbalances, thyroid function, or infections.
Treatment Options for Bradycardia
Treatment depends on the underlying cause and severity of symptoms. Common interventions include:
Lifestyle Adjustments
- Reducing stress and avoiding stimulants.
- Managing underlying health conditions such as hypertension or diabetes.
Medical Management
- Medication Review: Adjusting or discontinuing drugs that may cause bradycardia.
- Pacemaker Implantation: A device that regulates heart rhythm in severe cases.
- Treatment for Underlying Conditions: Managing thyroid disorders or electrolyte imbalances.
Preventing Bradycardia
While not all cases are preventable, these strategies can reduce the risk:
- Regular Health Checkups: Monitor heart health and catch issues early.
- Heart-Healthy Lifestyle: Engage in regular exercise, maintain a balanced diet, and avoid tobacco and excessive alcohol.
- Medication Awareness: Be informed about the potential side effects of medications.
- Managing Sleep Apnea: Seek treatment for sleep disorders to improve overall health.
When to Seek Medical Attention
Seek immediate medical care if you experience severe symptoms such as chest pain, fainting, or shortness of breath. Early intervention can prevent complications and improve outcomes.
Bradycardia is a complex condition with a range of causes and manifestations. Understanding its symptoms and underlying factors is crucial for timely diagnosis and treatment. By adopting a heart-healthy lifestyle and staying informed, individuals can better manage or prevent the complications associated with this condition.

