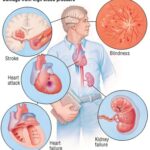
Distributive shock is a life-threatening condition characterized by severe vasodilation, resulting in inadequate blood flow to organs. Hypotension is a primary symptom, requiring prompt diagnosis and treatment to prevent organ failure and death.

Pathophysiology of Distributive Shock
Distributive shock disrupts the normal distribution of blood due to vascular dilation and increased permeability. The primary causes include:
- Sepsis: The most common cause, driven by bacterial endotoxins triggering widespread inflammation.
- Anaphylaxis: Severe allergic reactions causing rapid vasodilation.
- Neurogenic Shock: Caused by spinal cord injuries disrupting sympathetic tone.
- Endocrine Disorders: Conditions such as adrenal insufficiency can reduce vascular tone.
Mechanism of Hypotension in Distributive Shock
The underlying mechanism involves:
- Vasodilation: Widening of blood vessels reduces systemic vascular resistance (SVR).
- Capillary Leakage: Fluid shift from vessels to tissues decreases circulating blood volume.
- Myocardial Depression: In septic conditions, toxins may impair heart contractility.
Clinical Signs and Symptoms
Patients with distributive shock may present with:
- Hypotension (systolic BP < 90 mmHg)
- Warm, flushed skin initially
- Tachycardia and weak pulse
- Reduced urine output
- Altered mental status
Diagnosis of Hypotension Due to Distributive Shock
A thorough assessment combining clinical examination and diagnostic tools is vital.
Key Diagnostic Measures:
- Vital Signs Monitoring: Continuous tracking of blood pressure and heart rate.
- Blood Tests: To identify infection markers, electrolyte imbalances, and lactate levels.
- Echocardiography: Evaluates heart function and detects myocardial depression.
- Central Venous Pressure (CVP) Measurement: Determines fluid status.
Treatment Strategies for Hypotension in Distributive Shock
Effective treatment requires addressing the underlying cause and stabilizing hemodynamics.
1. Fluid Resuscitation
- Crystalloids such as saline or lactated Ringer’s solution are the first-line treatment.
- Colloids may be used in specific cases of severe fluid loss.
2. Vasopressor Therapy
- Norepinephrine is the preferred vasopressor to restore vascular tone.
- Epinephrine may be added in cases of septic or anaphylactic shock.
3. Antibiotic Therapy
- Broad-spectrum antibiotics should be initiated promptly in suspected sepsis cases.
4. Corticosteroids
- Administered in refractory shock cases, particularly in adrenal insufficiency.
5. Oxygen and Ventilatory Support
- Ensuring adequate oxygenation is critical for maintaining organ function.
Prognosis and Recovery
Outcomes vary depending on the underlying cause, severity, and timing of intervention. Early recognition and aggressive management improve survival rates significantly.
Prevention and Risk Reduction
- Vaccination against common bacterial pathogens reduces sepsis risk.
- Prompt Allergy Management minimizes anaphylactic shock occurrences.
- Careful Monitoring in ICU settings is crucial for high-risk patients.
FAQs
Q1: What is the primary treatment for hypotension in septic shock?
Fluid resuscitation combined with vasopressors such as norepinephrine is the primary treatment strategy.
Q2: How can hypotension in anaphylaxis be managed?
Epinephrine administration is the first-line treatment, followed by fluid resuscitation and antihistamines.
Q3: What are the early warning signs of distributive shock?
Warm, flushed skin, tachycardia, and confusion are common early indicators.
Q4: How does sepsis lead to hypotension?
Sepsis triggers widespread vasodilation, fluid leakage, and myocardial dysfunction, contributing to hypotension.
Q5: What diagnostic tests confirm distributive shock?
Blood tests, echocardiography, and lactate monitoring are key diagnostic tools.