Hypogammaglobulinemia is an immunodeficiency disorder characterized by abnormally low levels of immunoglobulins, increasing susceptibility to recurrent bacterial infections. This condition can be primary (genetic) or secondary (acquired), impacting immune defense mechanisms.

Causes of Hypogammaglobulinemia
- Primary Immunodeficiency Disorders: X-linked agammaglobulinemia, Common Variable Immunodeficiency (CVID), and selective IgA deficiency.
- Secondary Causes: Chronic lymphocytic leukemia (CLL), multiple myeloma, immunosuppressive therapies, and malnutrition.
- Medications: Prolonged corticosteroid use or chemotherapy.
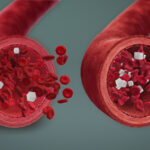
Pathophysiology of Hypogammaglobulinemia
In hypogammaglobulinemia, B cells may fail to produce sufficient antibodies, impairing immune response. The following diagram illustrates the mechanism:
Symptoms of Hypogammaglobulinemia
- Frequent respiratory tract infections (sinusitis, bronchitis, pneumonia)
- Chronic gastrointestinal infections
- Persistent skin infections
- Joint pain and fatigue
Diagnosis of Hypogammaglobulinemia
- Serum Immunoglobulin Tests: Measure levels of IgG, IgA, and IgM.
- Flow Cytometry: Assesses B-cell population and functionality.
- Genetic Testing: Identifies inherited immunodeficiency disorders.
- Vaccination Response Tests: Evaluates immune response to immunization.
Treatment for Hypogammaglobulinemia
- Immunoglobulin Replacement Therapy (IVIG/SCIG): Restores antibody levels to prevent infections.
- Antibiotic Prophylaxis: Continuous low-dose antibiotics to reduce infection risks.
- Vaccinations: Pneumococcal, influenza, and meningococcal vaccines are recommended.
- Management of Underlying Conditions: Addressing secondary causes like hematologic disorders or medication adjustments.
Preventive Strategies for Recurrent Infections
- Good Hygiene Practices: Reduces bacterial exposure.
- Regular Immunological Assessments: Ensures timely treatment adjustments.
- Lifestyle Modifications: Balanced nutrition and exercise can enhance immune resilience.
Complications of Untreated Hypogammaglobulinemia
- Chronic Lung Disease: Frequent respiratory infections can cause bronchiectasis.
- Autoimmune Disorders: Increased risk of conditions such as rheumatoid arthritis or lupus.
- Organ Damage: Persistent bacterial infections can lead to organ dysfunction.
Prognosis and Long-Term Outlook
With timely diagnosis and effective management, individuals with hypogammaglobulinemia can lead relatively normal lives. Ongoing monitoring and preventive care are crucial for minimizing complications.
FAQs
Q1: What is the most common symptom of hypogammaglobulinemia?
Frequent respiratory infections, such as sinusitis or pneumonia, are common indicators.
Q2: Can hypogammaglobulinemia be cured?
While there is no definitive cure, effective management through immunoglobulin therapy and preventive strategies can significantly improve quality of life.
Q3: Is hypogammaglobulinemia hereditary?
Some forms, such as X-linked agammaglobulinemia, are genetic, while others result from environmental factors or medical conditions.
Q4: How is hypogammaglobulinemia different from agammaglobulinemia?
Hypogammaglobulinemia involves low antibody levels, while agammaglobulinemia is characterized by a complete absence of antibodies.
Q5: Can children develop hypogammaglobulinemia?
Yes, primary immunodeficiency disorders can manifest in early childhood, necessitating early intervention.