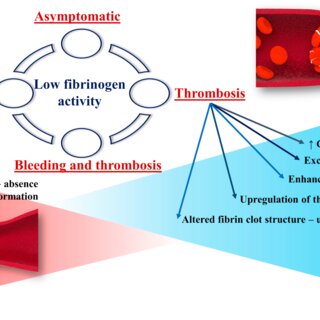
Hypofibrinogenemia is a rare blood disorder characterized by abnormally low levels of fibrinogen, a critical protein involved in blood clotting. This condition can lead to excessive bleeding, delayed clot formation, and increased risk of hemorrhage.
What is Hypofibrinogenemia?
Fibrinogen, also known as Factor I, is an essential protein in the coagulation cascade. Hypofibrinogenemia occurs when fibrinogen levels fall below the normal range of 200-400 mg/dL. This condition can be congenital (inherited) or acquired (developed due to other medical conditions).
Types of Hypofibrinogenemia
1. Congenital Hypofibrinogenemia
- Caused by genetic mutations in the FGA, FGB, or FGG genes.
- Typically presents with mild bleeding symptoms but may lead to severe bleeding episodes under stress, surgery, or injury.
2. Acquired Hypofibrinogenemia
- Often linked to liver disease, disseminated intravascular coagulation (DIC), or fibrinolytic therapy.
- Can develop in patients undergoing significant trauma, sepsis, or severe burns.
Causes of Hypofibrinogenemia
- Genetic Mutations: Congenital cases result from mutations affecting fibrinogen production or structure.
- Liver Disease: As fibrinogen is synthesized in the liver, conditions like cirrhosis or hepatitis may impair its production.
- Disseminated Intravascular Coagulation (DIC): This serious condition depletes fibrinogen during excessive clotting events.
- Massive Blood Transfusions: Dilution of blood components can reduce fibrinogen levels.
- Fibrinolytic Therapy: Medications such as tissue plasminogen activator (tPA) may lower fibrinogen levels.
Symptoms of Hypofibrinogenemia
Symptoms vary in severity depending on fibrinogen levels and may include:
- Easy bruising
- Prolonged bleeding from minor injuries
- Heavy menstrual bleeding
- Gastrointestinal bleeding
- Post-surgical bleeding
- Spontaneous joint or muscle bleeding
Diagnosis of Hypofibrinogenemia
Accurate diagnosis involves a combination of clinical assessment and laboratory tests:
Key Diagnostic Tests
- Fibrinogen Activity Test (Clauss Method): Measures fibrinogen function in the blood.
- Fibrinogen Antigen Test: Evaluates the amount of fibrinogen present.
- Prothrombin Time (PT): Assesses blood clotting time.
- Activated Partial Thromboplastin Time (aPTT): Identifies clotting abnormalities.
- Thrombin Time (TT): Detects issues related to fibrinogen function.
Treatment of Hypofibrinogenemia
Treatment depends on the severity and underlying cause of the condition:
1. Fibrinogen Replacement Therapy
- Cryoprecipitate: Rich in fibrinogen, used in acute bleeding episodes.
- Fibrinogen Concentrates: Preferred for long-term management due to precise dosing.
2. Fresh Frozen Plasma (FFP)
- Effective in emergency settings when fibrinogen concentrates are unavailable.
3. Managing Underlying Conditions
- Treating liver disease, controlling DIC, or modifying fibrinolytic therapy is crucial in acquired hypofibrinogenemia cases.
Complications of Hypofibrinogenemia
If untreated, hypofibrinogenemia can lead to:
- Severe bleeding episodes
- Post-surgical complications
- Miscarriage or excessive postpartum bleeding in pregnant women
Preventive Measures and Management
- Genetic counseling for families with congenital hypofibrinogenemia history.
- Regular monitoring of fibrinogen levels for high-risk patients.
- Prompt treatment of underlying conditions such as liver disease or DIC.
Prognosis and Outlook
With appropriate diagnosis and treatment, most patients with hypofibrinogenemia can manage their condition effectively. Early intervention minimizes severe bleeding risks and improves long-term outcomes.
Frequently Asked Questions:
Q1: Is hypofibrinogenemia a life-threatening condition?
A: Severe cases can be life-threatening without proper treatment, particularly during surgery or trauma.
Q2: Can hypofibrinogenemia be cured?
A: While congenital cases are lifelong conditions, acquired hypofibrinogenemia may improve with treatment of the underlying cause.
Q3: What foods can help improve fibrinogen levels?
A: While diet alone cannot cure hypofibrinogenemia, foods rich in omega-3, vitamin K, and iron may support overall blood health.
Q4: How is hypofibrinogenemia different from afibrinogenemia?
A: Hypofibrinogenemia refers to low fibrinogen levels, while afibrinogenemia indicates an absence of fibrinogen.
Q5: Are there any lifestyle modifications for managing hypofibrinogenemia?
A: Patients should avoid contact sports, monitor bleeding risks, and maintain routine medical check-ups.