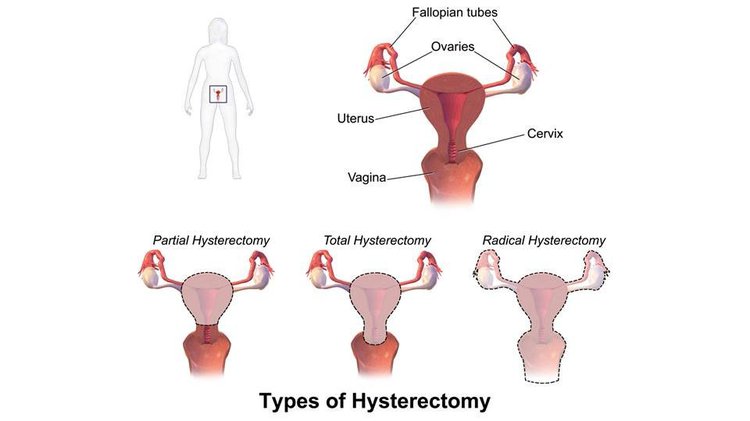
Bilateral oophorectomy, the surgical removal of both ovaries, leads to an abrupt decline in estrogen levels. This significant hormonal change results in hypoestrogenism, which can have profound effects on physical, emotional, and sexual well-being.
Understanding Hypoestrogenism
Hypoestrogenism refers to a deficiency of estrogen, a crucial hormone in regulating various bodily functions. Estrogen is essential for maintaining bone density, cardiovascular health, and the female reproductive system. The sudden drop in estrogen after a bilateral oophorectomy can trigger numerous symptoms and long-term health risks.
Causes of Hypoestrogenism Post-Oophorectomy
Surgical Indications for Bilateral Oophorectomy
- Cancer Treatment: Removal of ovaries may be necessary in cases of ovarian, uterine, or breast cancer.
- Genetic Risk Factors: Women with BRCA1 or BRCA2 mutations may opt for preventive oophorectomy.
- Endometriosis Management: In severe cases, bilateral oophorectomy may be recommended to control the condition.
- Pelvic Infections or Cysts: Extensive infection or cyst formation may necessitate ovarian removal.
Hormonal Impact
The abrupt cessation of ovarian function results in an immediate and significant estrogen deficiency, unlike natural menopause where hormonal decline occurs gradually.
Symptoms of Hypoestrogenism After Bilateral Oophorectomy
Immediate Symptoms
- Hot Flashes and Night Sweats: These vasomotor symptoms are common and often severe.
- Vaginal Dryness and Atrophy: Estrogen maintains vaginal tissue elasticity and lubrication.
- Mood Swings and Depression: Sudden hormonal shifts can impact mental health.
- Sleep Disturbances: Insomnia or restless sleep is prevalent.
Long-Term Health Risks
- Osteoporosis: Estrogen is crucial for bone density; deficiency accelerates bone loss.
- Cardiovascular Issues: Estrogen plays a protective role in heart health.
- Cognitive Decline: Estrogen’s neuroprotective effects may impact memory and cognition.
Diagnosis of Hypoestrogenism Post-Oophorectomy
Clinical Evaluation
- Medical History Assessment: Understanding the patient’s surgical background and symptoms.
- Physical Examination: Detecting signs such as vaginal atrophy, dry skin, and brittle hair.
Hormonal Tests
- Estradiol Levels: A critical indicator of estrogen status.
- FSH and LH Tests: Elevated levels often confirm estrogen deficiency.
Treatment Strategies for Hypoestrogenism
Hormone Replacement Therapy (HRT)
- Estrogen-Only Therapy: Recommended for women without a uterus.
- Combined HRT: Estrogen-progestin therapy for those with an intact uterus to reduce endometrial cancer risk.
Non-Hormonal Treatments
- Vaginal Moisturizers and Lubricants: For vaginal dryness and irritation.
- Antidepressants: Selective serotonin reuptake inhibitors (SSRIs) may alleviate mood disturbances and hot flashes.
- Bone Health Supplements: Calcium, vitamin D, and bisphosphonates support bone density.
Lifestyle Modifications
- Balanced Diet: Rich in calcium and phytoestrogens (e.g., soy products).
- Regular Exercise: Weight-bearing exercises help maintain bone density.
- Stress Management: Yoga, meditation, and mindfulness can improve mood and well-being.
Prevention Strategies
Risk Assessment
- Genetic Testing: BRCA mutation testing for high-risk individuals.
- Alternative Therapies: In some cases, conservative surgical options may preserve ovarian function.
Early Intervention
- Bone Density Monitoring: Early detection of osteoporosis risk.
- Cardiovascular Screening: Regular checks to prevent heart-related complications.
Hypoestrogenism resulting from bilateral oophorectomy poses significant health challenges. Timely diagnosis, appropriate hormone therapy, and lifestyle adjustments can mitigate risks and improve quality of life. Patients should consult healthcare providers for personalized treatment strategies to manage estrogen deficiency effectively.
FAQs
What is the primary cause of hypoestrogenism after bilateral oophorectomy?
The primary cause is the abrupt removal of estrogen-producing ovaries, which leads to immediate estrogen deficiency.
How long do symptoms of hypoestrogenism last?
Symptoms can persist for months or even years without treatment. Hormone replacement therapy often helps alleviate symptoms effectively.
Can hypoestrogenism increase cancer risk?
While estrogen therapy can carry some risks, managed treatment under medical supervision generally minimizes complications.
What lifestyle changes can help manage hypoestrogenism?
A healthy diet, regular exercise, and stress reduction techniques can significantly improve symptoms and long-term well-being.
Is hormone replacement therapy safe for all patients?
HRT suitability varies based on individual health profiles. Consulting a healthcare provider is crucial before starting therapy.