Bronchiolitis obliterans with organizing pneumonia (BOOP), also known as cryptogenic organizing pneumonia (COP), is a rare inflammatory condition affecting the small airways (bronchioles) and alveoli in the lungs. Unlike infectious pneumonia, BOOP is not caused by a pathogen but results from abnormal tissue repair processes leading to fibrosis and inflammatory changes within the lung parenchyma.
This article provides an in-depth analysis of BOOP, covering its clinical features, diagnostic criteria, underlying causes, treatment modalities, and prognosis.
Pathophysiology of BOOP
BOOP is characterized by the formation of granulation tissue plugs in the lumens of small airways, alveolar ducts, and alveoli. These plugs are composed of fibroblasts and myofibroblasts embedded in a matrix of connective tissue. The underlying mechanism involves excessive repair of epithelial injury, leading to uncontrolled fibroproliferation and inflammation. Over time, this can result in impaired gas exchange and reduced lung function.
Causes and Risk Factors
BOOP can occur idiopathically (cryptogenic organizing pneumonia) or secondary to specific triggers. Understanding potential causes is crucial for tailoring treatment approaches.
Idiopathic Causes
- Cryptogenic organizing pneumonia (COP) is a form of BOOP with no identifiable cause, accounting for most cases.
Secondary Causes
- Infections: Viral, bacterial, or fungal infections can trigger BOOP.
- Medications: Certain drugs, including chemotherapy agents, amiodarone, and methotrexate, have been implicated.
- Autoimmune Diseases: Conditions like rheumatoid arthritis, lupus, and dermatomyositis increase susceptibility.
- Toxins and Irritants: Prolonged exposure to toxic fumes, dust, or smoke.
- Radiation Therapy: Particularly in patients undergoing treatment for breast or lung cancer.
Clinical Presentation
Patients with BOOP may present with diverse respiratory and systemic symptoms. Common features include:
- Respiratory Symptoms: Persistent cough, shortness of breath, and wheezing.
- Systemic Symptoms: Fever, fatigue, weight loss, and night sweats.
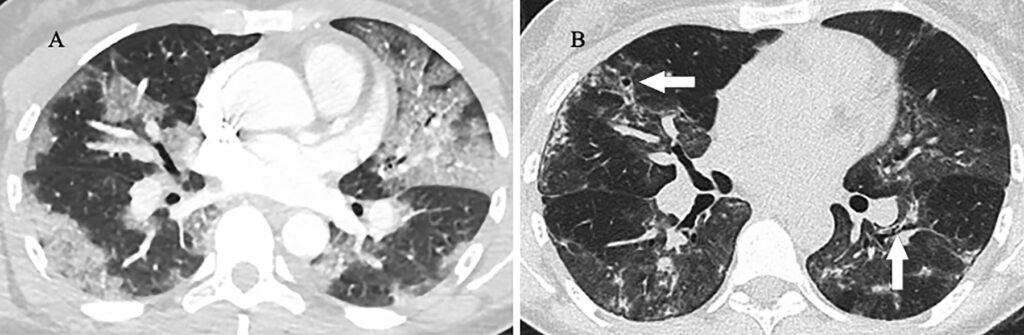
- Radiological Findings: Bilateral patchy lung opacities often visible on chest X-rays and CT scans.
Diagnostic Criteria
Diagnosing BOOP requires a thorough clinical evaluation supported by imaging studies and histopathological confirmation.
Diagnostic Steps
- Clinical Assessment: Detailed medical history and physical examination.
- Imaging Studies: High-resolution CT scans showing bilateral patchy consolidations, ground-glass opacities, and nodular patterns.
- Pulmonary Function Tests (PFTs): Restrictive ventilatory defect with decreased diffusion capacity.
- Bronchoscopy and Biopsy: Tissue samples confirming granulation tissue in airways and alveoli.
Treatment Strategies
Effective management of BOOP relies on addressing the underlying cause (if identifiable) and mitigating inflammation.
First-Line Treatment
- Corticosteroids: Prednisone is the most commonly prescribed medication, often leading to significant symptom improvement within weeks.
Secondary Treatments
- Immunosuppressive Agents: In cases unresponsive to corticosteroids, drugs like azathioprine or cyclophosphamide may be used.
- Supportive Care: Oxygen therapy for hypoxemia and pulmonary rehabilitation to improve functional capacity.
Monitoring and Relapse Management
Regular follow-up with pulmonary specialists is essential, as relapses are common. Tapering corticosteroids too quickly may lead to recurrence of symptoms.
Prognosis and Long-Term Outlook
Negative Predictors: Presence of comorbidities and delayed diagnosis.
Positive Predictors: Early intervention and good response to corticosteroids.
BOOP generally has a favorable prognosis when diagnosed early and treated appropriately. However, delayed treatment or severe cases can lead to chronic lung disease or respiratory failure.
Bronchiolitis obliterans with organizing pneumonia (BOOP) is a rare yet treatable condition. Prompt diagnosis and appropriate management are critical to improving outcomes. Continued research and patient education are essential for better understanding and addressing this condition.