Hypocalcemia is a common and serious electrolyte disturbance in patients with end-stage renal disease (ESRD) undergoing dialysis. This condition arises due to multiple factors, including impaired calcium regulation, vitamin D deficiency, and altered parathyroid hormone (PTH) dynamics. Timely diagnosis and management are crucial to prevent severe complications.
Causes of Hypocalcemia in ESRD with Dialysis
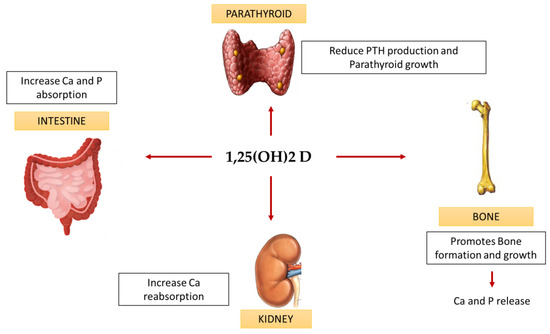
1. Impaired Vitamin D Activation
Patients with ESRD have reduced kidney function, impairing the conversion of inactive vitamin D into its active form, calcitriol. This deficiency lowers calcium absorption in the intestines, contributing to hypocalcemia.
2. Secondary Hyperparathyroidism
In ESRD, declining calcium levels stimulate excess PTH secretion to compensate. However, in prolonged conditions, this leads to bone resorption and calcium imbalance.
3. Phosphate Retention
ESRD patients commonly experience phosphate retention, which binds calcium in the bloodstream, reducing its bioavailability and contributing to hypocalcemia.
4. Dialysis-Related Factors
Dialysis processes can inadvertently lower calcium levels. Certain dialysate compositions may contain low calcium concentrations, exacerbating hypocalcemia.
5. Calcium-Sensing Receptor (CaSR) Dysfunction
In ESRD patients, altered CaSR function can impair calcium balance, leading to persistent hypocalcemia despite treatment.
Symptoms of Hypocalcemia in Dialysis Patients
Hypocalcemia can present with various symptoms, ranging from mild to severe:
- Muscle cramps and spasms
- Numbness and tingling (paresthesia)
- Cardiac arrhythmias
- Seizures
- Tetany (involuntary muscle contractions)
- Cognitive disturbances such as confusion and memory impairment
Diagnostic Approach for Hypocalcemia in ESRD
1. Serum Calcium Measurement
Total calcium and ionized calcium levels should be assessed to confirm hypocalcemia.
2. Parathyroid Hormone (PTH) Levels
Elevated PTH levels indicate secondary hyperparathyroidism, a common cause in ESRD patients.
3. Serum Phosphate and Magnesium
Assessing these electrolytes helps identify related imbalances contributing to hypocalcemia.
4. Vitamin D Status
Evaluating calcitriol levels can reveal vitamin D deficiency, requiring supplementation.
5. Dialysate Calcium Concentration
Monitoring dialysate composition ensures optimal calcium levels during dialysis.
Management of Hypocalcemia in Dialysis Patients
1. Calcium Supplementation
- Oral Calcium Carbonate or Acetate: Commonly used to increase calcium levels and control phosphate.
- Intravenous Calcium Gluconate: Administered in severe hypocalcemia cases or acute symptomatic conditions.
2. Vitamin D Supplementation
Activated vitamin D analogs such as calcitriol or paricalcitol are prescribed to improve calcium absorption.
3. Phosphate Binders
Phosphate control agents like sevelamer or lanthanum carbonate reduce phosphate retention, indirectly improving calcium balance.
4. Dialysate Calcium Adjustment
Modifying calcium concentration in the dialysate can stabilize serum calcium levels.
5. Managing Secondary Hyperparathyroidism
Medications such as cinacalcet or parathyroidectomy may be required for uncontrolled hyperparathyroidism.
Complications of Untreated Hypocalcemia in ESRD
If left untreated, hypocalcemia can lead to severe complications such as:
- Osteomalacia and fractures
- Cardiovascular instability
- Seizures and life-threatening tetany
Preventive Measures
- Regular monitoring of calcium, phosphate, and PTH levels.
- Ensuring optimal dialysate composition.
- Adherence to prescribed medications for calcium and vitamin D management.
Managing hypocalcemia in ESRD patients undergoing dialysis requires a comprehensive approach that includes calcium and phosphate regulation, vitamin D supplementation, and dialysate adjustments. By understanding the underlying causes and adopting a proactive management strategy, healthcare providers can improve patient outcomes and reduce complications.

