Hypocalcemia associated with hypoparathyroidism is a condition characterized by low calcium levels in the blood due to insufficient parathyroid hormone (PTH) production. This disorder requires prompt diagnosis and appropriate management to prevent serious complications.
Understanding Hypoparathyroidism
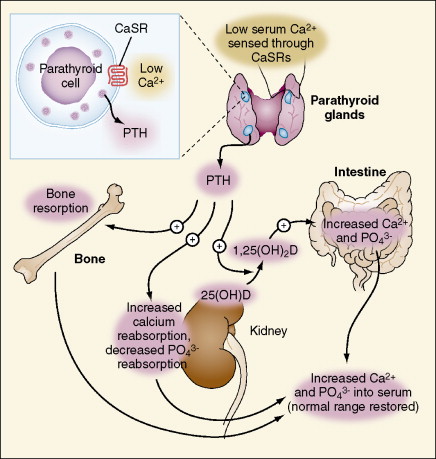
Hypoparathyroidism occurs when the parathyroid glands fail to produce adequate PTH. Since PTH plays a critical role in calcium regulation, its deficiency directly results in hypocalcemia.
Causes of Hypocalcemia in Hypoparathyroidism
- Post-surgical hypoparathyroidism: The most common cause, often resulting from thyroid or parathyroid gland surgery.
- Autoimmune conditions: Autoimmune destruction of parathyroid glands can impair PTH secretion.
- Genetic disorders: Conditions like DiGeorge syndrome or activating mutations in the calcium-sensing receptor (CaSR) gene.
- Infiltrative diseases: Sarcoidosis or iron overload may damage parathyroid glands.
- Radiation therapy: Radiation exposure in the neck region may impair parathyroid function.
Pathophysiology of Hypocalcemia in Hypoparathyroidism
PTH is essential for calcium homeostasis. Its absence results in reduced calcium resorption from bones, decreased calcium absorption in the intestines, and impaired calcium reabsorption in the kidneys. Consequently, serum calcium levels decline, triggering symptoms of hypocalcemia.
Clinical Symptoms of Hypocalcemia
Symptoms range from mild to severe, depending on calcium levels. Key symptoms include:
- Neuromuscular symptoms: Muscle cramps, tetany, and paresthesia.
- Cognitive symptoms: Brain fog, confusion, and memory issues.
- Cardiac complications: Prolonged QT interval, arrhythmias, and heart failure.
- Skin and hair changes: Dry skin, brittle nails, and hair thinning.
- Ocular issues: Cataract formation in chronic cases.
Diagnosis of Hypocalcemia
Diagnosis involves laboratory and clinical assessments:
- Serum calcium levels: Total and ionized calcium levels.
- PTH levels: Typically low in hypoparathyroidism.
- Phosphorus levels: Often elevated in this condition.
- Magnesium levels: Hypomagnesemia may exacerbate hypocalcemia.
- Electrocardiogram (ECG): Evaluates cardiac abnormalities linked to hypocalcemia.
Treatment Strategies for Hypocalcemia in Hypoparathyroidism
Effective treatment involves calcium restoration and maintaining stable levels.
1. Calcium Supplements
- Oral calcium carbonate or calcium citrate supplements are commonly prescribed.
- Intravenous calcium gluconate is administered in acute cases.
2. Vitamin D Therapy
- Active vitamin D analogs such as calcitriol or alfacalcidol improve calcium absorption.
3. Magnesium Supplementation
- Magnesium correction is crucial, especially in hypomagnesemia-induced hypocalcemia.
4. Parathyroid Hormone Replacement
- Recombinant PTH analogs like teriparatide or rhPTH (1-84) provide effective hormone replacement.
5. Dietary Modifications
- Increasing dietary calcium intake through dairy, green vegetables, and fortified foods supports calcium levels.
Potential Complications
Untreated or poorly managed hypocalcemia can lead to:
- Seizures
- Laryngospasm
- Heart failure
- Calcification of soft tissues
- Osteosclerosis and skeletal abnormalities
Prognosis and Long-term Management
With appropriate treatment and monitoring, most patients achieve stable calcium levels. Regular assessments, including serum calcium, PTH, and renal function, are vital in long-term management.
FAQs
Q1. What is the primary cause of hypocalcemia in hypoparathyroidism?
Post-surgical hypoparathyroidism following thyroidectomy or neck surgery is the leading cause.
Q2. Can dietary changes alone correct hypocalcemia in hypoparathyroidism?
Dietary modifications help but are often insufficient without calcium and vitamin D supplementation.
Q3. Are there any permanent treatments for hypocalcemia in hypoparathyroidism?
Recombinant PTH therapy offers a long-term solution for persistent cases.
Q4. How can I prevent complications of hypocalcemia?
Adhering to prescribed medications, dietary adjustments, and regular monitoring minimizes risks.
Q5. What are the risks of untreated hypocalcemia?
Untreated hypocalcemia can lead to life-threatening conditions like seizures and cardiac complications.