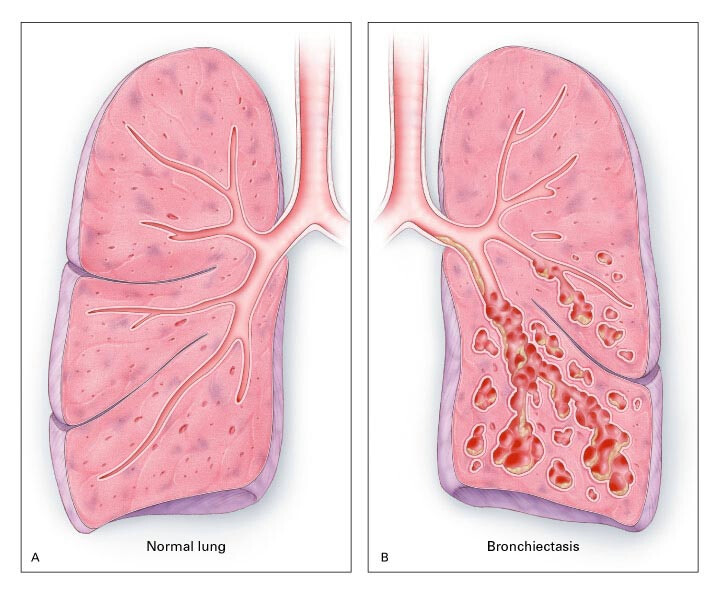
Bronchiectasis is a chronic lung condition characterized by the irreversible widening of the airways (bronchi), leading to persistent mucus buildup and recurrent infections. This condition can significantly impact respiratory health and overall quality of life. In this comprehensive guide, we will explore the causes, symptoms, diagnostic methods, treatment options, and management strategies for bronchiectasis.
What is Bronchiectasis?
Bronchiectasis occurs when the walls of the bronchi are damaged due to chronic inflammation or infection. This damage impairs the ability of the airways to clear mucus, creating an environment conducive to bacterial growth and repeated infections. Over time, this cycle exacerbates airway damage.
Causes of Bronchiectasis
Understanding the underlying causes of bronchiectasis is essential for effective management. The condition can result from a variety of factors, including:
- Infections: Severe or repeated respiratory infections, such as pneumonia, tuberculosis, or whooping cough.
- Immune System Disorders: Conditions like common variable immunodeficiency (CVID) or chronic granulomatous disease.
- Congenital Disorders: Genetic conditions such as cystic fibrosis or primary ciliary dyskinesia.
- Obstruction: Blockages in the airways due to tumors, foreign objects, or impacted mucus.
- Inflammatory Conditions: Diseases such as rheumatoid arthritis or Crohn’s disease.
Symptoms of Bronchiectasis
Symptoms of bronchiectasis can vary in severity and often worsen over time if untreated. Common signs include:
- Chronic cough producing thick sputum
- Recurrent chest infections
- Shortness of breath
- Wheezing
- Fatigue
- Chest pain
- Clubbing of fingers (in advanced cases)
How is Bronchiectasis Diagnosed?
Diagnosis typically involves a combination of clinical evaluation, imaging studies, and laboratory tests. The following methods are commonly used:
- Medical History and Physical Exam: Identifying recurrent respiratory infections or underlying conditions.
- High-Resolution CT Scan (HRCT): The gold standard for visualizing airway dilation and structural damage.
- Pulmonary Function Tests (PFTs): Assessing lung function and the extent of airway obstruction.
- Sputum Analysis: Identifying infectious agents or inflammatory markers.
- Blood Tests: Checking for immune deficiencies or other systemic conditions.
Treatment Options for Bronchiectasis
Managing bronchiectasis focuses on controlling symptoms, preventing infections, and slowing disease progression. Treatment strategies include:
1. Medications
- Antibiotics: To treat and prevent infections.
- Bronchodilators: To open airways and improve breathing.
- Mucolytics: To thin mucus and facilitate clearance.
- Anti-inflammatory Drugs: To reduce airway inflammation.
2. Airway Clearance Techniques
- Chest Physiotherapy: Manual techniques to loosen mucus.
- Positive Expiratory Pressure (PEP) Devices: To aid mucus clearance.
- Inhalation Therapy: Using nebulizers for medication delivery.
3. Surgery
In severe cases, surgical intervention such as lung resection may be necessary to remove damaged tissue or address localized bronchiectasis.
4. Vaccinations
Ensuring up-to-date vaccinations against influenza and pneumococcal infections can reduce the risk of complications.
Living with Bronchiectasis
Long-term management involves lifestyle modifications and regular monitoring. Key strategies include:
- Smoking Cessation: Avoiding tobacco to prevent further lung damage.
- Regular Exercise: Improving lung capacity and overall health.
- Healthy Diet: Supporting the immune system with balanced nutrition.
- Hydration: Aiding mucus clearance with adequate fluid intake.
- Pulmonary Rehabilitation: Participating in programs to enhance respiratory function.
Complications of Bronchiectasis
Untreated bronchiectasis can lead to serious complications, such as:
- Recurrent lung infections
- Respiratory failure
- Hemoptysis (coughing up blood)
- Pulmonary hypertension
Its a complex condition requiring a multidisciplinary approach for effective management. By understanding its causes, symptoms, and treatment options, patients and healthcare providers can work together to improve outcomes and enhance quality of life. Early diagnosis and adherence to treatment plans are critical in preventing complications and preserving lung function.
MYHEALTHMAG