Hyperparathyroidism secondary to chronic renal failure, also known as secondary hyperparathyroidism (SHPT), is a common complication in patients with long-term kidney disease. This condition arises due to the kidneys’ inability to maintain calcium, phosphorus, and vitamin D balance, triggering excessive parathyroid hormone (PTH) production. Early detection and effective management are crucial to prevent severe bone, cardiovascular, and systemic complications.
Pathophysiology of Secondary Hyperparathyroidism
Secondary hyperparathyroidism results from disturbances in the body’s calcium-phosphorus balance caused by chronic renal failure. The key mechanisms include:
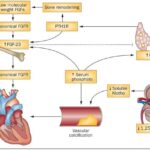
- Phosphate Retention: Impaired renal excretion leads to hyperphosphatemia, reducing serum calcium levels and stimulating PTH secretion.
- Vitamin D Deficiency: Diseased kidneys fail to convert 25-hydroxyvitamin D into its active form, calcitriol, impairing calcium absorption in the gut.
- Calcium Sensing Receptor Dysfunction: Persistent hypocalcemia reduces the sensitivity of the calcium-sensing receptors in the parathyroid glands, leading to increased PTH secretion.
Clinical Presentation
Patients with secondary hyperparathyroidism may experience:
- Bone Pain and Fractures: Due to impaired bone mineralization.
- Calciphylaxis: Vascular calcification causing ischemia and skin necrosis.
- Muscle Weakness and Fatigue: Resulting from mineral imbalances.
- Pruritus (Itching): A common symptom in patients with end-stage renal disease.
Diagnostic Criteria
Accurate diagnosis requires:
- Serum Calcium Levels: Typically low to normal.
- Serum Phosphorus Levels: Often elevated.
- PTH Levels: Significantly elevated.
- Vitamin D Levels: Frequently deficient.
- Bone Mineral Density (BMD): May show signs of osteoporosis or osteomalacia.
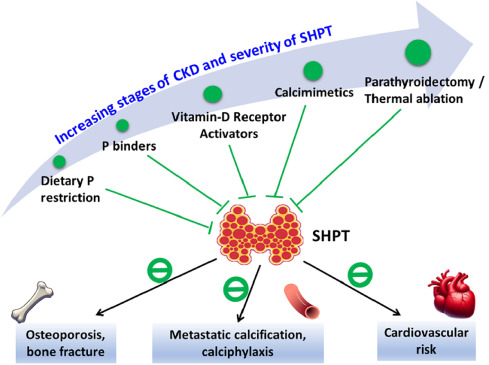
Treatment Strategies
Effective management of hyperparathyroidism secondary to chronic renal failure involves:
1. Phosphate Control
- Dietary Phosphate Restriction: Limiting high-phosphorus foods like dairy, processed meats, and soda.
- Phosphate Binders: Such as calcium carbonate, calcium acetate, or non-calcium-based agents like sevelamer and lanthanum carbonate.
2. Vitamin D Supplementation
- Active Vitamin D Analogues: Such as calcitriol, alfacalcidol, or paricalcitol to enhance calcium absorption and reduce PTH secretion.
3. Calcimimetics
- Cinacalcet: A medication that increases the calcium-sensing receptor’s sensitivity, lowering PTH levels effectively.
4. Parathyroidectomy
- Surgical Intervention: Recommended for patients with severe or refractory hyperparathyroidism to remove hyperplastic parathyroid glands.
Preventive Measures
To minimize the risk of developing SHPT in patients with chronic renal failure:
- Regular Monitoring: Routine checks for calcium, phosphorus, and PTH levels.
- Dietary Management: Focus on a balanced diet to control phosphate intake.
- Early Intervention: Prompt treatment with vitamin D analogues and phosphate binders can prevent severe complications.
Complications of Untreated SHPT
Neglected secondary hyperparathyroidism may result in:
- Renal Osteodystrophy: Bone deformities and fractures.
- Cardiovascular Disease: Due to vascular calcification.
- Soft Tissue Calcification: Leading to painful and disfiguring lesions.
Secondary hyperparathyroidism is a significant concern in patients with chronic renal failure. Timely diagnosis and comprehensive treatment are essential to mitigate complications and improve quality of life. Close collaboration between nephrologists, endocrinologists, and dietitians plays a vital role in successful management.
FAQs
Q1: What is the primary cause of hyperparathyroidism in chronic renal failure?
A1: Phosphate retention, vitamin D deficiency, and calcium-sensing receptor dysfunction are key factors.
Q2: How can SHPT be prevented in CKD patients?
A2: Early intervention with phosphate binders, vitamin D analogues, and dietary control can help prevent SHPT.
Q3: What are the risks of untreated SHPT?
A3: Untreated SHPT can lead to severe bone disease, cardiovascular issues, and calciphylaxis.
Q4: Is surgery necessary for all SHPT cases?
A4: Surgery is typically reserved for severe or treatment-resistant cases.
Q5: Are there specific dietary recommendations for SHPT management?
A5: Limiting phosphate-rich foods and maintaining balanced calcium intake is crucial for management.