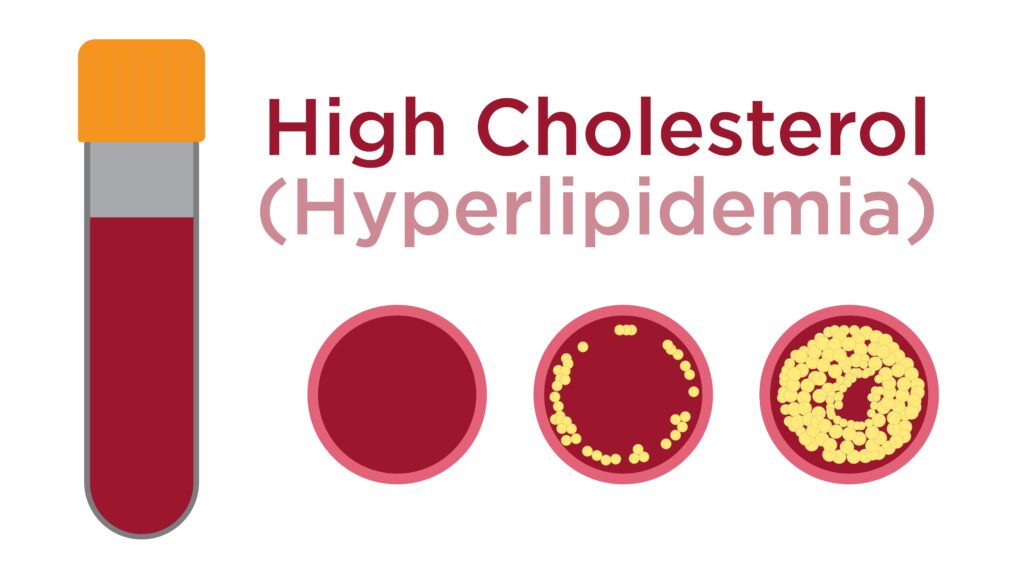
Hyperlipidemia is a medical condition characterized by elevated levels of lipids (fats) in the blood, notably cholesterol and triglycerides. This condition significantly increases the risk of cardiovascular diseases such as heart attacks and strokes.
Types of Hyperlipidemia
Hyperlipidemia can be classified into several categories based on lipid abnormalities:
- Primary Hyperlipidemia: Genetically inherited conditions that affect lipid metabolism.
- Secondary Hyperlipidemia: Caused by lifestyle factors, obesity, or medical conditions such as diabetes and hypothyroidism.
- Mixed Hyperlipidemia: A combination of elevated cholesterol and triglycerides.
Causes of Hyperlipidemia
Key causes include:
- Poor Diet: High intake of saturated fats, trans fats, and refined sugars.
- Sedentary Lifestyle: Lack of physical activity can contribute to high lipid levels.
- Genetics: Familial hypercholesterolemia is a hereditary condition linked to elevated cholesterol.
- Medical Conditions: Diabetes, kidney disease, and thyroid disorders can influence lipid levels.
- Medications: Certain drugs like steroids and diuretics may elevate cholesterol.
Symptoms of Hyperlipidemia
Hyperlipidemia often presents no clear symptoms in its early stages. However, prolonged elevation can result in:
- Fatty deposits around the eyes (xanthelasma)
- Abnormal skin patches (xanthomas)
- Chest pain or heart-related complications in severe cases
Risk Factors
Several factors elevate the risk of developing hyperlipidemia:
- Age: Risk increases with age.
- Genetics: Family history of hyperlipidemia.
- Obesity: Excess body weight is strongly linked to abnormal lipid levels.
- Smoking: Damages blood vessels, making cholesterol buildup easier.
Diagnosis
Diagnosis involves a lipid profile test, which measures:
- Total Cholesterol: Ideal levels should be below 200 mg/dL.
- LDL (Low-Density Lipoprotein) Cholesterol: Often called “bad cholesterol,” LDL should be less than 100 mg/dL.
- HDL (High-Density Lipoprotein) Cholesterol: Known as “good cholesterol,” HDL levels should exceed 60 mg/dL.
- Triglycerides: Optimal levels should be below 150 mg/dL.
Treatment and Management
1. Lifestyle Modifications
- Healthy Diet: Emphasize fruits, vegetables, whole grains, and healthy fats like omega-3.
- Regular Exercise: Aim for at least 150 minutes of moderate-intensity activity per week.
- Weight Management: Maintaining a healthy BMI can improve cholesterol levels.
- Smoking Cessation: Reduces cardiovascular risks significantly.
2. Medications
For persistent or severe cases, medications may be necessary:
- Statins: Most common drugs for lowering LDL cholesterol.
- Fibrates: Effective for reducing triglycerides.
- Bile Acid Sequestrants: Help the body eliminate cholesterol.
- PCSK9 Inhibitors: Powerful medications for patients with genetic hyperlipidemia.
3. Natural Remedies and Supplements
Certain supplements may aid in controlling cholesterol levels:
- Omega-3 Fatty Acids: Found in fish oils to reduce triglycerides.
- Niacin: Effective in raising HDL cholesterol.
- Fiber Supplements: Help improve digestion and manage cholesterol.
Complications of Untreated
Uncontrolled hyperlipidemia can lead to serious health concerns:
- Atherosclerosis: Hardening and narrowing of the arteries.
- Heart Attack: Resulting from blocked coronary arteries.
- Stroke: Due to reduced blood supply to the brain.
- Peripheral Artery Disease (PAD): Blocked arteries affecting limbs.
Prevention Strategies for Hyperlipidemia
Preventive measures include:
- Regular lipid profile screenings.
- Adopting a heart-healthy diet.
- Staying physically active and maintaining a healthy weight.
- Managing chronic conditions like diabetes and hypertension.
FAQs:
What foods should I avoid with it?
Avoid processed foods, fried items, full-fat dairy, and sugary treats.
Can hyperlipidemia be reversed?
With consistent lifestyle changes and medication adherence, cholesterol levels can often be significantly improved.
Is hyperlipidemia hereditary?
Yes, familial hypercholesterolemia is an inherited form of hyperlipidemia requiring specialized treatment.
How often should I check my cholesterol levels?
Adults should undergo a lipid profile test every 4-6 years or more frequently if at risk.
Can exercise alone reduce cholesterol levels?
While exercise is crucial, combining it with dietary changes and medications (if prescribed) yields the best results.
By understanding hyperlipidemia’s causes, symptoms, and treatment options, individuals can take proactive steps to improve their cardiovascular health.