Hyperinsulinism is a medical condition characterized by excessive insulin production in the body. This condition often results in hypoglycemia (low blood sugar), which can lead to severe complications if left untreated. Hyperinsulinism is commonly seen in newborns and children but may also affect adults.
Types of Hyperinsulinism: Hyperinsulinism Causes
1. Congenital Hyperinsulinism (CHI)
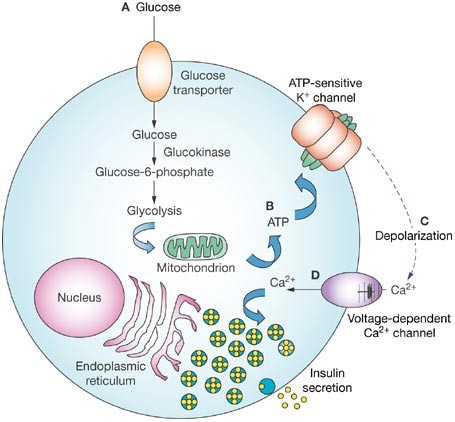
Congenital hyperinsulinism is a genetic disorder resulting in unregulated insulin secretion from pancreatic beta cells. It is the most common cause of persistent hypoglycemia in infants and can vary in severity.
2. Acquired Hyperinsulinism
Acquired hyperinsulinism typically occurs due to pancreatic tumors (insulinomas), medication side effects, or metabolic imbalances.
Causes of Hyperinsulinism
Several factors can contribute to excessive insulin production, including:
- Genetic mutations affecting beta-cell regulation (common in congenital hyperinsulinism).
- Pancreatic tumors such as insulinomas.
- Metabolic disorders disrupting glucose regulation.
- Certain medications like sulfonylureas or quinine.
- Post-gastric bypass surgery leading to excessive insulin release after meals.
Symptoms of Hyperinsulinism
Signs of hyperinsulinism can range from mild to severe and may include:
- Persistent or severe hypoglycemia
- Weakness, fatigue, or dizziness
- Irritability and confusion
- Rapid heartbeat and sweating
- Seizures or unconsciousness in extreme cases
- Developmental delays in infants
Diagnosis of Hyperinsulinism
A comprehensive diagnosis requires a combination of medical history, physical examination, and laboratory tests. Diagnostic procedures may include:
- Blood tests to measure glucose and insulin levels.
- Fasting tests to assess glucose control under monitored conditions.
- Imaging scans such as CT or MRI to identify insulinoma or pancreatic abnormalities.
- Genetic testing for suspected congenital hyperinsulinism.
Treatment Options for Hyperinsulinism
1. Medical Treatment
- Diazoxide is commonly prescribed to inhibit insulin release.
- Octreotide injections may help control severe hypoglycemia.
- Glucagon injections are used to counteract low blood sugar emergencies.
2. Dietary Management
- Frequent, small, carbohydrate-rich meals can stabilize blood sugar levels.
- Continuous glucose monitoring devices can help track fluctuations effectively.
3. Surgical Intervention
- Partial pancreatectomy is performed in severe congenital hyperinsulinism.
- Insulinoma removal is the primary treatment for tumor-induced hyperinsulinism.
Long-Term Management and Prognosis
Patients with hyperinsulinism often require lifelong monitoring to prevent complications. Early diagnosis and proper management significantly improve outcomes. For infants with congenital hyperinsulinism, consistent glucose monitoring and dietary control are crucial for healthy development.
FAQs
What is the primary cause of congenital hyperinsulinism?
Congenital hyperinsulinism is primarily caused by genetic mutations affecting insulin regulation in pancreatic beta cells.
Can adults develop hyperinsulinism?
Yes, adults may develop hyperinsulinism, often due to insulinomas or certain medications.
Is hyperinsulinism life-threatening?
Severe cases can be life-threatening without prompt treatment, particularly when associated with persistent hypoglycemia.
How is hyperinsulinism managed in infants?
Infants often require a combination of medications, glucose infusions, and specialized feeding plans.
Are there lifestyle changes to prevent hyperinsulinism?
Maintaining a balanced diet, managing stress, and regular medical check-ups can help prevent acquired forms of hyperinsulinism.