Hyperfibrinolysis-induced hemorrhage is a critical condition characterized by excessive fibrinolytic activity, leading to severe and uncontrolled bleeding. This condition often arises in response to trauma, surgery, or specific medical disorders that disrupt normal hemostasis.
Pathophysiology of Hyperfibrinolysis
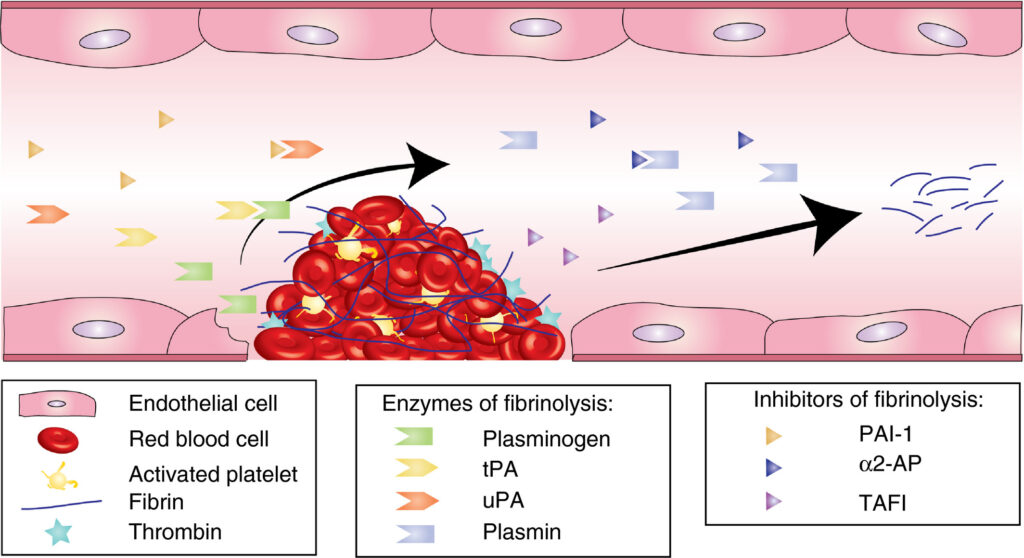
Hyperfibrinolysis occurs when fibrinolytic enzymes, such as plasmin, degrade fibrin clots excessively, compromising blood clot stability. This results in increased bleeding risk due to impaired clot formation and fibrin degradation.
Key Mechanisms of Hyperfibrinolysis
- Primary Hyperfibrinolysis: Direct activation of plasminogen into plasmin without prior coagulation involvement.
- Secondary Hyperfibrinolysis: Triggered by extensive clotting processes, frequently seen in trauma or surgery.
Causes and Risk Factors
Several conditions can induce hyperfibrinolysis, including:
- Severe trauma and hemorrhagic shock
- Major surgeries, particularly cardiac and hepatic procedures
- Disseminated intravascular coagulation (DIC)
- Liver dysfunction
- Cancer-related coagulopathy
- Certain medications, such as thrombolytic agents
Symptoms and Clinical Presentation
Symptoms vary depending on the severity of the condition. Common signs include:
- Persistent bleeding from wounds or surgical sites
- Excessive bruising and hematoma formation
- Mucosal bleeding (e.g., gums and nose)
- Hematuria and gastrointestinal bleeding
Diagnostic Approaches
Prompt diagnosis is crucial for managing hyperfibrinolysis-induced hemorrhage. Common diagnostic tools include:
- Thromboelastography (TEG): Detects abnormal fibrinolysis patterns.
- Rotational Thromboelastometry (ROTEM): Provides detailed insights into coagulation and fibrinolysis.
- D-dimer Assay: Elevated levels indicate excessive fibrinolysis.
- Plasmin-Antiplasmin Complex Testing: Identifies active plasmin production.
Treatment Strategies
Effective treatment aims to stabilize clot formation and suppress excessive fibrinolysis.
Antifibrinolytic Agents
- Tranexamic Acid (TXA): Reduces plasminogen activation and fibrin degradation.
- Epsilon-Aminocaproic Acid (EACA): Inhibits plasmin formation.
Supportive Therapies
- Blood product transfusions: Administering fresh frozen plasma (FFP) and cryoprecipitate to restore clotting factors.
- Recombinant Factor VIIa: Used in severe cases to control bleeding.
- Correction of underlying conditions: Treating liver dysfunction, DIC, or other causative factors.
Prevention and Risk Management
- Early identification in trauma or surgery patients.
- Proactive administration of TXA in high-risk cases.
- Close monitoring using TEG/ROTEM in critical care settings.
Prognosis and Outcomes
With timely intervention, the prognosis for patients with hyperfibrinolysis-induced hemorrhage improves significantly. Delayed treatment may result in extensive blood loss, organ damage, and increased mortality rates.
Hyperfibrinolysis-induced hemorrhage is a complex yet manageable condition. Understanding its pathophysiology, identifying risk factors, and utilizing targeted therapies are essential to improving patient outcomes. Early intervention, combined with effective diagnostic tools and appropriate medications, can significantly reduce bleeding risks and enhance recovery.