Hypercortisolism, also known as Cushing’s syndrome, is a medical condition characterized by excessive levels of cortisol in the body. Cortisol, a hormone produced by the adrenal glands, plays a vital role in regulating metabolism, blood pressure, and the immune response. Hypercortisolism can result from prolonged exposure to high cortisol levels, leading to a range of serious health complications.
Causes of Hypercortisolism
Hypercortisolism can be classified into endogenous and exogenous causes:
Endogenous Causes
- Pituitary Adenoma (Cushing’s Disease): A benign tumor in the pituitary gland causes excessive secretion of adrenocorticotropic hormone (ACTH), which stimulates cortisol production.
- Adrenal Tumors: Both benign and malignant adrenal tumors may cause excessive cortisol production.
- Ectopic ACTH Syndrome: Certain types of tumors outside the pituitary gland, such as lung or pancreatic tumors, may secrete ACTH, leading to high cortisol levels.
Exogenous Causes
- Prolonged Use of Corticosteroid Medications: Medications like prednisone or dexamethasone, often prescribed for inflammatory conditions, can result in hypercortisolism when used in high doses or over an extended period.
Symptoms of Hypercortisolism
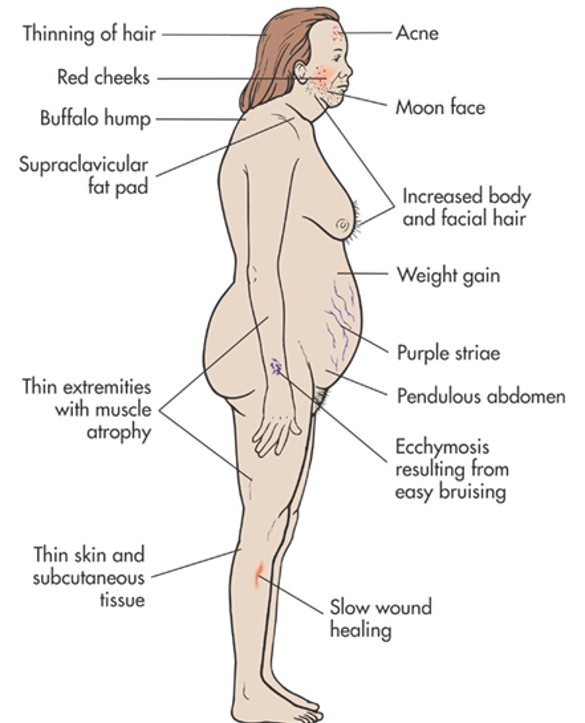
Hypercortisolism presents a range of symptoms that vary depending on the condition’s severity and duration. Common symptoms include:
- Weight Gain: Particularly in the face (moon face), abdomen, and upper back (buffalo hump).
- Skin Changes: Thinning skin, easy bruising, and purplish stretch marks (striae).
- Muscle Weakness: Particularly in the arms and legs.
- Osteoporosis: Fragile bones that are prone to fractures.
- Hypertension: Increased blood pressure levels.
- Mood Disorders: Depression, anxiety, and irritability.
- Increased Blood Sugar Levels: Risk of developing type 2 diabetes.
- Weakened Immune System: Greater susceptibility to infections.
Diagnosis of Hypercortisolism
Diagnosing hypercortisolism involves multiple tests to measure cortisol levels and determine its source. Common diagnostic procedures include:
- 24-hour Urine Free Cortisol Test: Measures cortisol levels in collected urine over a 24-hour period.
- Late-Night Salivary Cortisol Test: Evaluates cortisol secretion patterns, typically elevated in hypercortisolism.
- Dexamethasone Suppression Test: Measures how cortisol levels respond to synthetic steroid administration.
- Imaging Tests: MRI or CT scans help identify pituitary or adrenal tumors.
Treatment Options for Hypercortisolism
Treatment for hypercortisolism varies depending on its underlying cause:
Surgical Interventions
- Pituitary Surgery: Removal of pituitary adenomas through transsphenoidal surgery.
- Adrenalectomy: Surgical removal of adrenal tumors.
- Tumor Excision: Removal of ectopic ACTH-secreting tumors where applicable.
Medications
- Ketoconazole, Metyrapone, and Mitotane: Drugs that reduce cortisol production.
- Pasireotide: A medication that suppresses ACTH secretion in some cases.
Radiation Therapy
In cases where surgery is not effective, radiation therapy may be used to target pituitary tumors.
Lifestyle Modifications
- Balanced Diet: Emphasis on calcium, vitamin D, and protein intake to improve bone strength.
- Exercise Regimen: Regular physical activity to manage weight and improve overall health.
Potential Complications of Hypercortisolism
Untreated hypercortisolism can lead to severe complications, such as:
- Cardiovascular Disease: Elevated blood pressure and cholesterol levels increase heart disease risk.
- Osteoporosis-Related Fractures: Weakening of bones increases fracture susceptibility.
- Diabetes: Chronic hyperglycemia may develop.
- Psychiatric Disorders: Persistent mood swings, anxiety, and depression.
Preventive Measures for Hypercortisolism
While some causes of hypercortisolism cannot be prevented, certain steps may reduce the risk:
- Proper Medication Use: Follow prescribed corticosteroid dosage under medical supervision.
- Regular Health Screenings: Monitor cortisol levels for early detection in high-risk individuals.
- Healthy Lifestyle: Maintain a balanced diet, regular exercise, and stress management practices.
Prognosis and Recovery
Early diagnosis and appropriate treatment significantly improve the prognosis for individuals with hypercortisolism. Post-treatment recovery often involves managing potential side effects and addressing lifestyle factors to ensure long-term health.
FAQs
Q1: What is the most common cause of hypercortisolism?
A: Pituitary adenomas (Cushing’s disease) are the most common cause of endogenous hypercortisolism.
Q2: Can hypercortisolism be cured?
A: Yes, with proper treatment such as surgery, medication, or radiation therapy, hypercortisolism can often be managed or cured.
Q3: How does hypercortisolism affect mental health?
A: Hypercortisolism can cause mood swings, anxiety, depression, and cognitive issues.
Q4: Are there natural remedies for hypercortisolism?
A: While natural remedies like stress reduction techniques can support recovery, medical intervention is essential for treatment.
Q5: Is hypercortisolism life-threatening?
A: If untreated, hypercortisolism can lead to serious complications like heart disease and diabetes, making prompt diagnosis crucial.