Hypercalcemia, a condition characterized by elevated calcium levels in the blood, is commonly associated with primary hyperparathyroidism (PHPT). This endocrine disorder occurs due to excessive secretion of parathyroid hormone (PTH) from one or more enlarged or overactive parathyroid glands. Understanding its causes, symptoms, diagnosis, and treatment options is crucial for effective management.
Causes of Hypercalcemia in Primary Hyperparathyroidism
Primary hyperparathyroidism arises from several underlying conditions:
- Parathyroid Adenoma: A benign tumor in one of the parathyroid glands, responsible for over 85% of PHPT cases.
- Parathyroid Hyperplasia: Enlargement of multiple parathyroid glands, often linked to genetic conditions such as multiple endocrine neoplasia (MEN) types 1 and 2.
- Parathyroid Carcinoma: A rare but serious cause of PHPT involving malignant growth in the parathyroid glands.
Pathophysiology of Hypercalcemia in PHPT
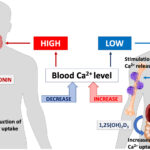
The excessive secretion of PTH results in:
- Increased Bone Resorption: PTH stimulates osteoclasts to break down bone tissue, releasing calcium into the bloodstream.
- Enhanced Renal Calcium Reabsorption: Elevated PTH reduces calcium excretion in the kidneys, further contributing to hypercalcemia.
- Increased Intestinal Calcium Absorption: PTH boosts vitamin D activation, enhancing calcium absorption from the intestines.
Symptoms of Hypercalcemia Due to PHPT
Symptoms can vary from mild to severe, often depending on calcium levels. Common symptoms include:
- Fatigue and Weakness
- Kidney Stones
- Bone Pain and Fractures
- Abdominal Discomfort
- Cognitive Impairment and Depression
- Frequent Urination and Thirst
- Nausea, Vomiting, and Constipation
Diagnosis of Hypercalcemia in PHPT
Accurate diagnosis involves a combination of clinical evaluation, biochemical tests, and imaging studies:
- Blood Tests: Elevated serum calcium and PTH levels are hallmark indicators.
- 24-Hour Urinary Calcium Test: Differentiates PHPT from familial hypocalciuric hypercalcemia (FHH).
- Bone Mineral Density Test: Identifies osteoporosis or bone loss linked to PHPT.
- Imaging Techniques: Ultrasound, Sestamibi scan, or CT scans help locate abnormal parathyroid glands.
Treatment Options for Hypercalcemia Due to PHPT
Surgical Intervention
Parathyroidectomy is the most effective treatment for PHPT. This procedure involves the removal of the overactive parathyroid gland(s). Minimally invasive techniques often yield quicker recovery and fewer complications.
Medical Management
For patients unable to undergo surgery, medications are employed to manage calcium levels:
- Bisphosphonates: Inhibit bone resorption to reduce calcium release.
- Calcimimetics (e.g., Cinacalcet): Lower PTH secretion and normalize calcium levels.
- Hydration and Diuretics: Increase calcium excretion through the kidneys.
Lifestyle Modifications
- Maintain adequate hydration.
- Engage in weight-bearing exercises to support bone health.
- Limit dietary calcium and vitamin D supplements unless prescribed.
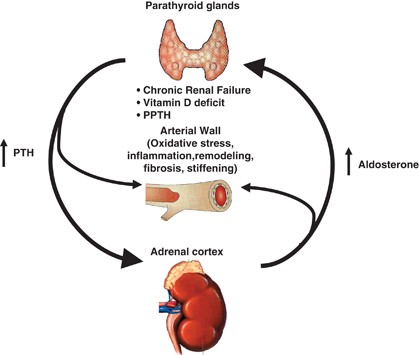
Complications of Untreated Hypercalcemia in PHPT
If left untreated, PHPT-induced hypercalcemia can lead to serious complications such as:
- Osteoporosis and Fractures
- Kidney Stones and Renal Impairment
- Cardiovascular Issues
- Neuropsychiatric Disorders
Prognosis and Long-Term Management
Following successful treatment, most patients experience improved calcium regulation and reduced symptoms. Regular follow-ups are essential to monitor calcium levels, bone health, and kidney function.
Hypercalcemia due to primary hyperparathyroidism is a significant medical concern requiring timely diagnosis and appropriate intervention. Understanding its causes, symptoms, and treatment options can help patients manage the condition effectively and prevent complications.
Frequently Asked Questions:
What is the most common cause of primary hyperparathyroidism?
Parathyroid adenoma is the most frequent cause, accounting for over 85% of cases.
Can primary hyperparathyroidism be treated without surgery?
Yes, medical management using drugs like calcimimetics or bisphosphonates can help control calcium levels, particularly in patients unfit for surgery.
What are the warning signs of severe hypercalcemia?
Severe fatigue, confusion, vomiting, and abnormal heart rhythms are key warning signs requiring immediate medical attention.
How can I prevent hypercalcemia if diagnosed with PHPT?
Staying hydrated, maintaining bone health, and following your healthcare provider’s recommendations are key preventive steps.
Is hypercalcemia reversible with treatment?
Yes, surgical removal of the affected gland(s) often results in complete calcium normalization.