Hypercalcemia associated with sarcoidosis is a medical condition characterized by elevated calcium levels in the blood due to the granulomatous inflammation seen in sarcoidosis. Understanding its causes, symptoms, and treatment options is essential for effective management.
What is Sarcoidosis?
Sarcoidosis is an inflammatory disease that causes granuloma formation in various organs, most commonly the lungs and lymph nodes. This immune response can lead to excessive production of vitamin D, resulting in hypercalcemia.
Causes of Hypercalcemia in Sarcoidosis
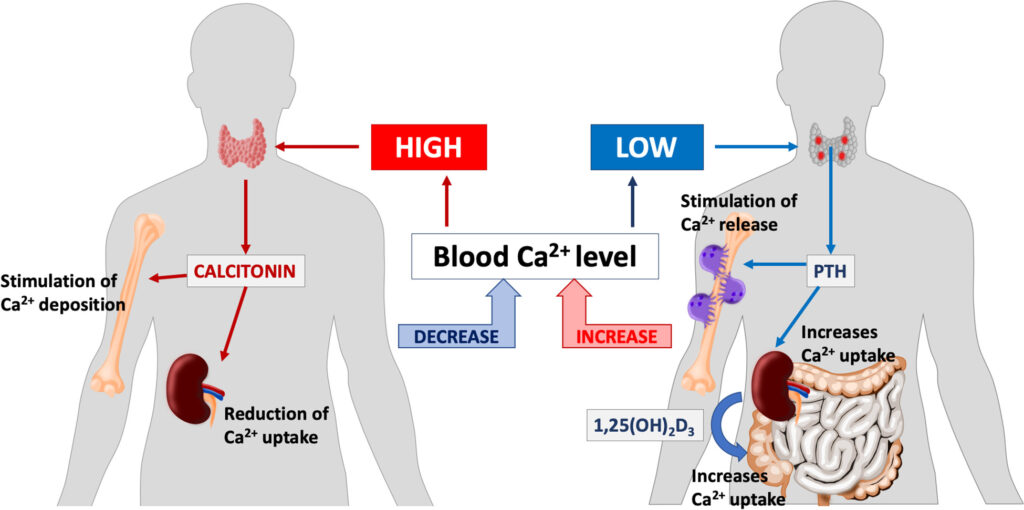
The primary cause of hypercalcemia in sarcoidosis is the overproduction of 1,25-dihydroxyvitamin D [1,25(OH)2D] by activated macrophages within granulomas. This excessive vitamin D leads to increased intestinal calcium absorption and elevated calcium levels in the blood.
Key Factors Contributing to Hypercalcemia
- Granulomatous Inflammation: Macrophages in granulomas convert inactive vitamin D to its active form, leading to calcium imbalances.
- Increased Calcium Absorption: Enhanced intestinal absorption of calcium due to elevated 1,25(OH)2D levels.
- Reduced Renal Calcium Excretion: Impaired calcium clearance by the kidneys may further elevate calcium levels.
Symptoms of Hypercalcemia in Sarcoidosis
Symptoms may range from mild to severe, depending on calcium levels. Common symptoms include:
- Fatigue and weakness
- Nausea and vomiting
- Constipation
- Abdominal pain
- Frequent urination and thirst
- Confusion, headaches, or altered mental status
- Muscle pain or bone discomfort
Severe cases may result in kidney stones, nephrocalcinosis, or cardiac arrhythmias.
Diagnosis of Hypercalcemia in Sarcoidosis
Diagnosis involves:
- Serum Calcium Test: Identifies elevated calcium levels.
- Vitamin D Metabolite Testing: Confirms increased 1,25(OH)2D levels.
- Chest X-ray/CT Scan: Detects granulomas in the lungs or lymph nodes.
- Serum Angiotensin-Converting Enzyme (ACE): Often elevated in sarcoidosis.
- Kidney Function Tests: Identifies potential renal complications.
Treatment Options for Hypercalcemia in Sarcoidosis
Effective treatment aims to reduce calcium levels and address the underlying inflammatory process.
Corticosteroids
- Prednisone is commonly prescribed to suppress inflammation and inhibit vitamin D production by macrophages.
Immunosuppressive Therapy
- Drugs such as methotrexate, azathioprine, or hydroxychloroquine may be used in severe cases.
Calcium and Vitamin D Regulation
- Dietary Calcium Restriction: Limiting calcium-rich foods may reduce serum calcium levels.
- Hydration Therapy: Adequate fluid intake promotes calcium excretion via the kidneys.
- Bisphosphonates: These medications help reduce calcium release from bones.
Severe Cases
For life-threatening hypercalcemia, options like calcitonin, denosumab, or dialysis may be required.
Preventive Measures
- Routine monitoring of calcium levels in sarcoidosis patients
- Early detection of symptoms associated with hypercalcemia
- Adequate hydration and balanced diet to prevent complications
FAQs
What causes hypercalcemia in sarcoidosis patients?
Hypercalcemia in sarcoidosis is caused by activated macrophages in granulomas producing excess 1,25-dihydroxyvitamin D, which enhances calcium absorption.
How is hypercalcemia in sarcoidosis diagnosed?
Diagnosis involves calcium level tests, vitamin D metabolite assessment, chest imaging, and kidney function evaluations.
Can hypercalcemia in sarcoidosis resolve on its own?
Mild cases may resolve with hydration and lifestyle adjustments; severe cases typically require medical intervention.
What are the risks of untreated hypercalcemia in sarcoidosis?
Untreated hypercalcemia may lead to kidney stones, nephrocalcinosis, bone loss, or cardiovascular complications.
Are corticosteroids effective in managing hypercalcemia in sarcoidosis?
Yes, corticosteroids are the primary treatment for reducing inflammation and controlling vitamin D overproduction.
Hypercalcemia associated with sarcoidosis is a manageable condition when diagnosed early and treated effectively. By addressing both calcium regulation and the underlying inflammatory process, patients can achieve improved outcomes and avoid serious complications.