Hyperammonemia due to methylmalonic acidemia (MMA) is a rare yet serious metabolic disorder characterized by elevated ammonia levels in the blood. This condition arises from a deficiency in enzymes crucial for amino acid metabolism, resulting in toxic accumulation of ammonia and organic acids.
Understanding Methylmalonic Acidemia (MMA)
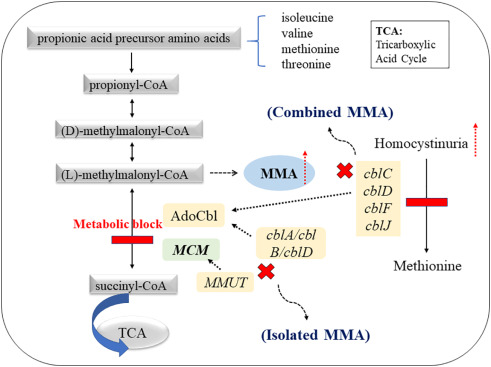
Methylmalonic acidemia is a genetic disorder caused by mutations in the MUT, MMAA, MMAB, MMACHC, or MMADHC genes. These mutations impair the body’s ability to break down certain fats and proteins, leading to the buildup of methylmalonic acid and subsequent metabolic complications.
Enzymatic Deficiency and Its Role in MMA
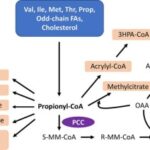
- MUT gene mutation: Leads to a deficiency in methylmalonyl-CoA mutase, an essential enzyme for processing specific amino acids.
- Cobalamin (Vitamin B12) Defect: Deficiencies in enzymes that process cobalamin can disrupt methylmalonyl-CoA mutase activity.
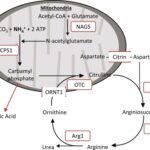
Pathophysiology of Hyperammonemia in MMA
The impaired metabolic pathways cause an accumulation of methylmalonic acid and ammonia. Ammonia toxicity results from the inability to effectively remove nitrogen waste products, affecting the central nervous system and leading to life-threatening consequences.
Symptoms of Hyperammonemia Due to MMA
Symptoms may vary based on the severity of the disorder but typically include:
- Neurological impairment (e.g., seizures, coma)
- Gastrointestinal symptoms (e.g., vomiting, feeding difficulties)
- Lethargy and weakness
- Developmental delays
- Metabolic crisis triggered by illness or fasting
Diagnosis of Hyperammonemia and MMA
Diagnostic Tests
- Plasma ammonia levels: Elevated ammonia concentrations confirm hyperammonemia.
- Blood gas analysis: Identifies acidosis linked to methylmalonic acid buildup.
- Urine organic acid analysis: Detects methylmalonic acid levels.
- Genetic testing: Confirms mutations in related genes for precise diagnosis.
Treatment Options for Hyperammonemia Due to MMA
Acute Management
- Intravenous glucose and lipids: To halt catabolism and reduce ammonia production.
- Ammonia scavengers: Medications like sodium benzoate and sodium phenylbutyrate aid ammonia removal.
- Hemodialysis: Utilized in severe cases to rapidly clear ammonia.
Long-Term Management
- Low-protein diet: Reduces ammonia production.
- Cobalamin (Vitamin B12) supplementation: Beneficial in patients with responsive MMA.
- Liver or combined liver-kidney transplantation: Effective in severe cases to improve metabolic stability.
Prognosis and Outcomes
The prognosis for individuals with MMA varies significantly depending on the severity and promptness of treatment. Early diagnosis, appropriate dietary management, and effective therapeutic interventions can improve long-term outcomes and reduce the risk of neurological damage.
Prevention and Genetic Counseling
Genetic counseling is crucial for families with a history of MMA. Prenatal diagnosis through amniocentesis or chorionic villus sampling (CVS) can help identify affected pregnancies.
Hyperammonemia due to methylmalonic acidemia is a life-threatening condition that demands immediate medical intervention. Understanding its genetic basis, symptoms, and available treatment strategies is essential for improving patient outcomes and preventing complications.