Hyperammonemia is a metabolic disorder characterized by elevated ammonia levels in the blood. Ammonia, a byproduct of amino acid metabolism, is typically converted to urea in the liver and excreted via the kidneys. Accumulation of ammonia can have severe neurological effects, making early diagnosis and intervention crucial.
Causes of Hyperammonemia
Hyperammonemia can result from genetic or acquired conditions. Key causes include:
Genetic Causes
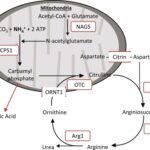
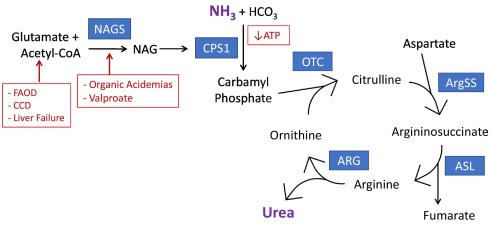
- Urea Cycle Disorders (UCDs): Inherited enzyme deficiencies impair the body’s ability to eliminate ammonia.
- Organic Acidemias: Disorders such as propionic acidemia and methylmalonic acidemia disrupt metabolic pathways, leading to ammonia buildup.
Acquired Causes
- Liver Dysfunction: Conditions like cirrhosis, hepatitis, and alcohol-induced liver damage impair ammonia detoxification.
- Medications: Certain drugs, particularly valproic acid, can induce hyperammonemia.
- Infections and Sepsis: Severe infections may elevate ammonia levels.
- Gastrointestinal Bleeding: Increased nitrogen load from digested blood may raise ammonia levels.
Symptoms of Hyperammonemia
Symptoms vary depending on ammonia concentration and the underlying cause. Common symptoms include:
- Altered mental status (confusion, disorientation)
- Lethargy and fatigue
- Vomiting
- Irritability
- Seizures
- Coma in severe cases
Diagnosis of Hyperammonemia
Early diagnosis is critical to prevent neurological damage. Diagnostic methods include:
Blood Tests
- Ammonia Levels: A serum ammonia test is the primary diagnostic tool.
- Liver Function Tests (LFTs): Evaluate liver performance to identify underlying hepatic dysfunction.
Imaging Studies
- CT Scans and MRI: Identify structural abnormalities in the brain resulting from ammonia toxicity.
Genetic Testing
- Recommended for individuals suspected of having urea cycle disorders or other metabolic conditions.
Treatment Options for Hyperammonemia
Treatment strategies aim to lower ammonia levels and address the underlying cause.
Immediate Interventions
- Intravenous Fluids and Glucose: Provides hydration and energy to stabilize metabolic processes.
- Ammonia-Lowering Agents: Medications such as sodium phenylbutyrate and sodium benzoate aid in ammonia detoxification.
- Hemodialysis: Used in severe cases for rapid ammonia clearance.
Long-Term Management
- Dietary Management: Low-protein diets combined with specialized supplements help reduce ammonia production.
- Liver Transplant: Recommended for individuals with severe liver dysfunction or refractory metabolic conditions.
Prevention of Hyperammonemia
Preventive strategies are essential for at-risk individuals:
- Routine Screening: Neonatal screening for urea cycle disorders enables early intervention.
- Genetic Counseling: Advisable for families with a history of metabolic conditions.
- Medication Monitoring: Close supervision of drugs known to elevate ammonia levels.
Prognosis and Outlook
Prognosis depends on the cause, ammonia levels, and treatment initiation. Early intervention generally improves outcomes, while untreated cases risk severe neurological damage or death.
Hyperammonemia is a serious medical condition requiring prompt diagnosis and management. By understanding its causes, symptoms, and treatment options, healthcare providers can improve patient outcomes through timely intervention and ongoing care.