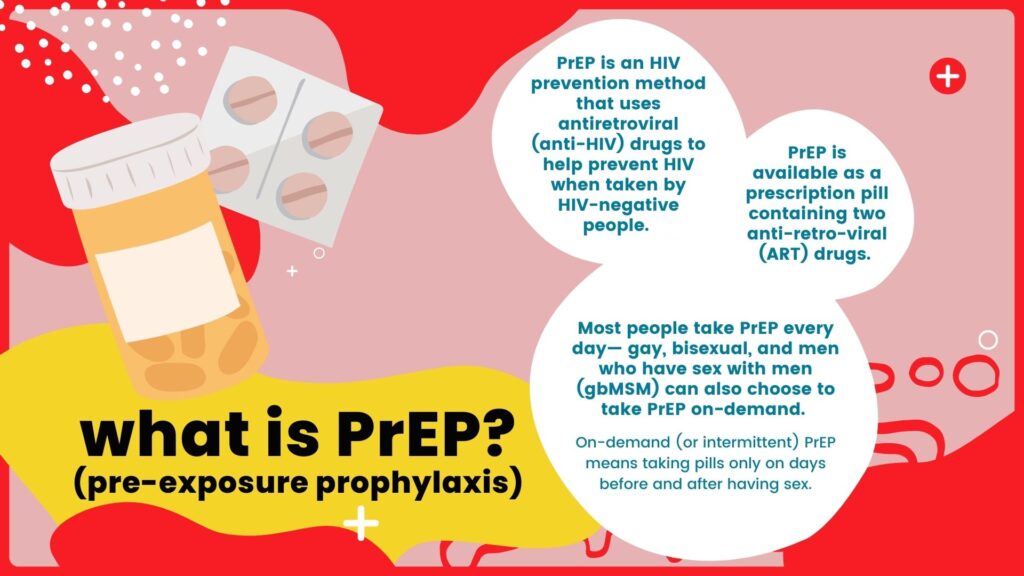
Pre-exposure prophylaxis (PrEP) is a powerful strategy for preventing HIV infection. This medical intervention involves taking antiretroviral medications to reduce the risk of contracting HIV in individuals who are HIV-negative but at high risk of exposure.
How Does PrEP Work?
PrEP medications contain two key antiretroviral drugs:
- Tenofovir disoproxil fumarate (TDF)
- Emtricitabine (FTC)
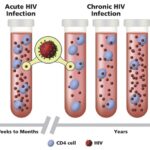
These medications prevent the HIV virus from establishing a permanent infection in the body by blocking the virus’s ability to replicate in healthy cells.
Who Should Consider PrEP?
PrEP is recommended for individuals who are HIV-negative but face an increased risk of infection. Key groups include:
- Individuals in sexual relationships with HIV-positive partners
- Men who have sex with men (MSM)
- Sex workers
- People who inject drugs
- Those with multiple sexual partners or inconsistent condom use
PrEP Effectiveness
When taken consistently, PrEP is highly effective:
- 99% effective in preventing HIV transmission through sexual activity.
- 74% effective in preventing transmission through injection drug use.
PrEP Medication Regimens
PrEP is available in daily pill form and as a long-acting injectable.
- Daily Oral PrEP: Common options include Truvada and Descovy.
- Injectable PrEP: Cabotegravir is an FDA-approved injectable administered every two months.
Side Effects and Risks
PrEP is generally well-tolerated, but some side effects may occur:
- Nausea
- Headaches
- Mild stomach discomfort
Serious side effects are rare but may include kidney problems or bone density loss. Regular monitoring by healthcare providers is essential.
PrEP and Pregnancy
PrEP can be safely used by individuals who are pregnant or breastfeeding, especially if they are at risk of HIV infection. Research shows no significant harm to the baby when PrEP is used appropriately under medical supervision.
Accessing PrEP
To start PrEP, individuals must:
- Consult a healthcare provider for HIV testing and risk assessment.
- Undergo routine follow-ups to monitor health status and ensure adherence.
- Obtain a prescription and adhere to the recommended regimen.
Cost and Insurance Coverage
PrEP may be covered by insurance or healthcare programs. Various support initiatives, such as Gilead’s Advancing Access Program, offer financial assistance to eligible individuals.
Myths and Misconceptions About PrEP
- Myth: PrEP is only for people who engage in high-risk behavior.
Fact: PrEP is recommended for anyone at risk of HIV exposure. - Myth: PrEP eliminates the need for condoms.
Fact: While PrEP is highly effective, condoms provide added protection against other sexually transmitted infections (STIs).
HIV infection pre-exposure prophylaxis (PrEP) is a vital tool in preventing HIV transmission. By offering robust protection and promoting safer sexual practices, PrEP empowers individuals to take proactive steps toward safeguarding their health.