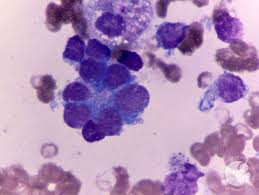
Neuroblastoma is a malignant tumor arising from neural crest cells, predominantly affecting children under five years of age. High-risk neuroblastoma, characterized by metastasis to bone and bone marrow, presents significant treatment challenges and is associated with poor prognosis. This article delves into the clinical characteristics, therapeutic approaches, and prognostic factors associated with high-risk neuroblastoma involving bone and bone marrow.
Clinical Characteristics
Patients with high-risk neuroblastoma often present with metastases to bone and bone marrow. A study involving 203 children with bone marrow metastasis reported the following metastatic sites at diagnosis:
- Bone: 96.1%
- Distant lymph nodes: 51.2%
- Skull and endomeninx: 30.0%
- Orbit: 14.8%
- Pleura: 7.9%
- Liver: 6.4%
- Canalis spinalis: 6.4%
- Other sites: 5.4%
- Skin and soft tissue: 4.9%
The median age at onset was 41 months, with a male predominance (58.1%).
Treatment Strategies
Management of high-risk neuroblastoma with bone and bone marrow involvement is multimodal, encompassing chemotherapy, surgery, radiation therapy, and autologous stem cell transplantation (ASCT). Emerging therapies, such as monoclonal antibodies targeting GD2, have shown promise. Notably, naxitamab, in combination with granulocyte-macrophage colony-stimulating factor (GM-CSF), received accelerated approval for pediatric patients aged one year and older with relapsed or refractory high-risk neuroblastoma in the bone or bone marrow. The recommended dosage is 3 mg/kg/day via intravenous infusion on days 1, 3, and 5 of each 4-week treatment cycle, alongside subcutaneous GM-CSF.
Prognostic Factors
Several factors influence the prognosis of high-risk neuroblastoma with bone and bone marrow involvement:
- MYCN Amplification: Identified as a poor prognostic indicator, MYCN amplification necessitates more aggressive treatment approaches.
- Age at Diagnosis: Patients older than 18 months exhibit a higher risk of bone marrow relapse, correlating with decreased survival rates.
- Metastatic Sites: Involvement of specific sites, such as the pleura, is associated with poorer outcomes.
- ASCT: Patients undergoing ASCT demonstrate significantly improved survival rates compared to those who do not receive transplantation.
Survival Outcomes
Despite intensive treatment, the prognosis for high-risk neuroblastoma with bone and bone marrow involvement remains guarded. The 5-year overall survival (OS) and event-free survival (EFS) rates are approximately 39.7% and 36.1%, respectively. Relapses are common, with bone marrow being the most frequent site. Patients receiving ASCT have better outcomes, highlighting the importance of incorporating transplantation into treatment protocols.
High-risk neuroblastoma involving bone and bone marrow presents significant therapeutic challenges. Advancements in multimodal treatment approaches, including the use of targeted therapies like naxitamab and the incorporation of ASCT, offer hope for improved outcomes. Ongoing research and clinical trials are essential to further enhance survival rates and quality of life for affected patients.

